Medex (Coumadin) vs Alternative Anticoagulants: Complete Comparison
 Oct, 17 2025
Oct, 17 2025
Anticoagulant Selection Tool
Personalized Anticoagulant Recommendation
This tool helps you understand which anticoagulant option might be best for you based on your specific medical situation. Please note: This is not a substitute for professional medical advice.
When it comes to preventing dangerous blood clots, dozens of drugs line the pharmacy shelves, but not all work the same way. Medex (Coumadin) is a long‑standing oral anticoagulant that belongs to the vitaminK antagonist family. Its active ingredient, warfarin, blocks the body's ability to recycle vitaminK, slowing down clot formation. While it has saved countless lives, newer agents-often called NOACs (non‑vitaminK antagonist oral anticoagulants)-promise fewer monitoring hassles and fewer food interactions. This guide walks you through the key differences, so you can see whether Coumadin alternatives might be a better fit for you or a loved one.
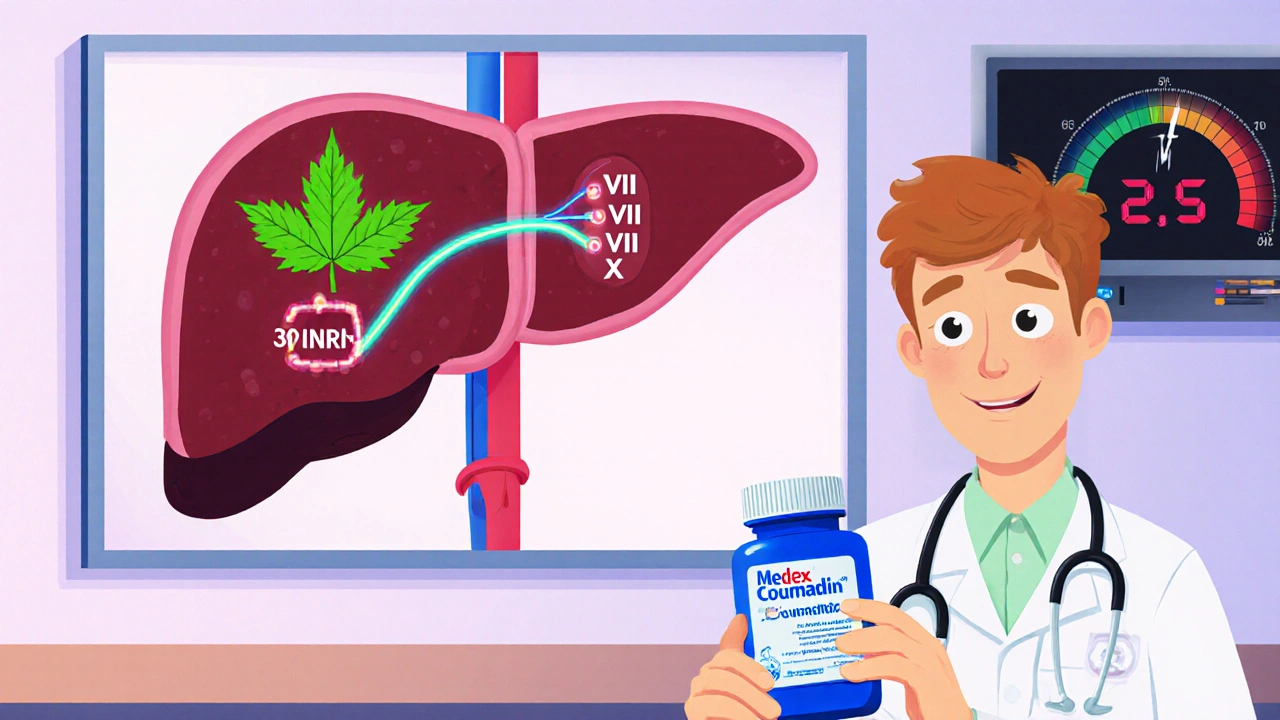
How Medex (Coumadin) Works
Medex (Coumadin) interferes with the liver's production of clotting factors II, VII, IX, and X. By reducing these proteins, the blood takes longer to clot. Because the effect depends on how much vitaminK you eat, doctors must frequently check the International Normalized Ratio (INR) to keep patients safely within a therapeutic range (usually 2.0‑3.0 for most indications).
Why Newer Anticoagulants Appeared
Warfarin (and by extension Medex) has been around since the 1950s, but its narrow therapeutic window and the need for regular blood tests made life tricky for many patients. In the early 2010s, four oral agents received FDA approval that target specific steps in the clotting cascade without needing vitaminK. These are commonly grouped under the term NOACs and include:
- Dabigatran (brand: Pradaxa)
- Rivaroxaban (brand: Xarelto)
- Apixaban (brand: Eliquis)
- Edoxaban (brand: Savaysa)
All of these work directly on thrombin or factorXa, making their action more predictable and often eliminating the need for routine INR checks.
Side‑Effect Profile Comparison
Bleeding is the most serious risk for any anticoagulant. Warfarin’s bleeding risk can be managed by adjusting the dose to keep the INR in range, but swings in diet or other medicines can cause sudden spikes. NOACs have a steadier pharmacokinetic profile, and clinical trials have shown slightly lower rates of intracranial hemorrhage. However, each drug has its own caveats:
- Dabigatran: Higher rates of gastrointestinal bleeding, especially at the 150mg dose.
- Rivaroxaban: Once‑daily dosing is convenient, but the drug is taken with food to improve absorption.
- Apixaban: Generally the safest NOAC for patients with kidney impairment.
- Edoxaban: Not recommended if the patient’s creatinine clearance is >95mL/min because efficacy drops.
Warfarin remains the go‑to for patients with mechanical heart valves or severe mitral stenosis, conditions where NOACs are not approved.
Monitoring and Lifestyle Considerations
With Medex (Coumadin), you’ll likely need weekly INR checks when you first start, then maybe monthly once stable. Diet matters-a lot. Green leafy vegetables (spinach, kale) are rich in vitaminK and can lower the drug’s effect. Alcohol can increase bleeding risk. In contrast, NOACs require no regular blood work and have minimal food interactions, freeing patients to eat a normal diet.
Reversal Options and Emergency Management
If bleeding occurs, doctors need a way to reverse the anticoagulant quickly. For warfarin, vitaminK infusion works, and there’s also prothrombin complex concentrate (PCC). For NOACs, specific reversal agents have been developed:
- Dabigatran: Idarucizumab (Praxbind)
- Rivaroxaban & Apixaban: Andexanet alfa (Andexxa)
- Edoxaban: Also uses Andexanet alfa
These agents are pricey, but they can stop life‑threatening bleeding within minutes.
Cost and Insurance Coverage
Cost is often the deciding factor. Warfarin itself is cheap-often under £5 a month-but the price of INR testing and clinic visits adds up. NOACs are more expensive upfront (roughly £100‑£150 per month in the UK) but eliminate the need for routine lab work. Many National Health Service (NHS) formularies now approve NOACs for atrial fibrillation, especially when patients struggle with warfarin management.
Side‑by‑Side Table of Key Attributes
| Attribute | Medex (Coumadin) | Dabigatran | Rivaroxaban | Apixaban | Edoxaban |
|---|---|---|---|---|---|
| Class | VitaminK antagonist | Direct thrombin inhibitor | FactorXa inhibitor | FactorXa inhibitor | FactorXa inhibitor |
| Typical dose | 2-10mg daily (adjusted) | 150mg twice daily | 20mg once daily (15mg if renal impairment) | 5mg twice daily (2.5mg if low weight) | 60mg once daily (30mg if renal impairment) |
| Monitoring | INR 2-3 | None | None | None | None |
| Reversal | VitaminK, PCC | Idarucizumab | Andexanet alfa | Andexanet alfa | Andexanet alfa |
| Half‑life | 36-42hours | 12-17hours | 5-9hours | 12hours | 10-14hours |
| Major interactions | VitaminK foods, many drugs | P‑glycoprotein inhibitors | Strong CYP3A4 inhibitors | Strong CYP3A4 inhibitors | Strong CYP3A4 inhibitors |
| Approved for | Atrial fibrillation, DVT/PE, prosthetic valve | A.Fib, DVT/PE | A.Fib, DVT/PE, post‑orthopedic surgery | A.Fib, DVT/PE | A.Fib, DVT/PE |

Choosing the Right Anticoagulant for You
There’s no one‑size‑fits‑all answer. If you have a mechanical heart valve, a history of severe liver disease, or you’re on medications that heavily interact with the cytochromeP450 system, Medex (Coumadin) might still be the safest bet. If you’re bothered by weekly blood draws and want a simpler regimen, a NOAC-especially Apixaban for patients with mild kidney issues-could be a better match.
Start the conversation with your cardiologist or hematologist. Ask about:
- Your specific clotting risk (stroke, DVT, PE)
- Kidney and liver function tests
- Potential drug‑drug and drug‑food interactions
- Insurance coverage and out‑of‑pocket costs
- Availability of reversal agents in case of emergency
Making an informed decision means weighing convenience against safety and cost against monitoring burden.
Common Myths About Warfarin and NOACs
Myth 1: Warfarin is “old” and therefore unsafe.
Reality: Decades of data show it’s highly effective when managed correctly. Errors usually stem from poor INR control, not the drug itself.
Myth 2: NOACs don’t need any monitoring.
Reality: While routine labs aren’t required, kidney function should be checked at least yearly because reduced clearance can build up drug levels.
Myth 3: All anticoagulants cost the same.
Reality: Warfarin cheap, but the hidden cost of INR clinics can make it comparable to NOACs over a year.
Quick Take‑Home Checklist
- Identify your primary indication (AFib, DVT, valve).
- Check kidney/liver labs before picking a drug.
- Consider lifestyle: diet restrictions vs. pill burden.
- Ask about reversal agents if you have high bleeding risk.
- Factor in total cost-including monitoring-for the long term.
Frequently Asked Questions
What is Medex (Coumadin) used for?
Medex (Coumadin) is prescribed to prevent and treat blood clots such as deep‑vein thrombosis (DVT), pulmonary embolism (PE), and to reduce stroke risk in atrial fibrillation. It’s also used in patients with mechanical heart valves.
How does a NOAC differ from warfarin?
NOACs target a single clotting factor (either thrombin or factorXa) and have a predictable effect, so they don’t require routine INR testing. Warfarin blocks vitaminK recycling, affecting several clotting factors, which makes dosing more variable and necessitates frequent monitoring.
Can I switch from Coumadin to a NOAC?
Yes, many clinicians transition patients once the INR is within therapeutic range. The exact overlap period depends on the chosen NOAC and kidney function, but the switch is usually safe under medical supervision.
What foods should I avoid while on Medex (Coumadin)?
Large amounts of leafy greens (spinach, kale, broccoli) are high in vitaminK and can lower Coumadin’s effect. Consistency is key-don’t quit these foods abruptly; instead, keep your intake steady and inform your doctor of any dietary changes.
Are there reversal agents for NOACs?
Yes. Dabigatran can be reversed with idarucizumab, while rivaroxaban, apixaban, and edoxaban can be countered with andexanet alfa. These agents are available in most major hospitals but can be costly.
Patricia Echegaray
October 17, 2025 AT 17:47Look, the whole “new‑fangled NOACs are safer” narrative is just a smokescreen cooked up by Big Pharma to keep us dependent on endless prescriptions and pricey patents. The moment you start whining about vitamin‑K veggies, you’re already in their trap, because they know the more you scramble to keep your INR steady, the deeper their cash flow goes. Warfarin’s cheap price tag and centuries‑old track record are proof that we don’t need a shiny pill to keep blood thin; we need a system that stops rewarding corporations for our misery.
Miriam Rahel
October 20, 2025 AT 15:14While the preceding observation raises an intriguing point, it overlooks the robust body of randomized controlled trials that have demonstrated a statistically significant reduction in intracranial hemorrhage with factor Xa inhibitors. Moreover, the pharmacokinetic predictability of NOACs obviates the need for frequent INR monitoring, thereby reducing healthcare utilization costs in the long term. It is therefore reductive to categorically dismiss these agents as mere “pharma ploys” without acknowledging the empirical evidence supporting their clinical efficacy.
Samantha Oldrid
October 23, 2025 AT 12:40Oh sure, because juggling blood tests and leafy greens is exactly the fun we all signed up for when we chose “warfarin”.
Malia Rivera
October 26, 2025 AT 09:07In the grand tapestry of medical progress, the shift from vitamin‑K antagonists to direct oral anticoagulants mirrors humanity’s perennial quest for convenience over contemplation. Yet, as we embrace these streamlined compounds, we must ask whether we are surrendering the nuanced art of personalized medicine on the altar of algorithmic simplicity.
lisa howard
October 29, 2025 AT 06:34When I first heard the term “NOAC” I imagined a sleek, futuristic weapon-something the government would hand out only to the elite, while the rest of us were left clutching warfarin like a relic from a bygone era. The reality, however, is far more theatrical. Imagine a patient strolling into the clinic, clutching a clipboard, waiting for the nurse to draw blood while the fluorescent lights hum ominously above-this has been the warfarin ritual for generations. Then, in a flash of marketing brilliance, the pharma giants rolled out dabigatran, rivaroxaban, apixaban, and edoxaban, each promising liberation from the tyranny of INR dots. The promise was seductive: “no more needles, no more diet restrictions, just one pill a day and you’re free!” Yet freedom, as any seasoned dramatist knows, comes with a price tag that would make a Hollywood blockbuster blush. The reversal agents-idarucizumab, andexanet alfa-are not just expensive; they are symbols of a healthcare system willing to gamble your life for profit margins. Patients who once measured their spinach intake now measure their bank accounts, calculating whether their insurance will cover the $150‑monthly pill or the $2000 reversal kit in case of a bleed. Doctors, caught between evidence‑based guidelines and the seductive allure of pharmaceutical sponsorships, find themselves navigating a labyrinth of conflicts of interest. The narrative is further complicated by the fact that warfarin remains the gold standard for mechanical heart valves, a niche that the NOACs simply cannot infiltrate. So while the newer agents shine like neon signs in the pharmacy aisles, older warfarin remains the steadfast, albeit temperamental, guardian for a subset of patients. In the end, the choice between warfarin and a NOAC is less about science and more about the theatrical production each side stages-complete with costumes, scripts, and a chorus of patients singing the praises of whichever drug they’ve been handed. And as the curtain rises on each clinical encounter, the audience-us, the patients-must decide whether we are merely actors in their commercial, or the directors of our own health destiny.
Cindy Thomas
November 1, 2025 AT 04:00Honestly, I think the hype around NOACs is overrated-sure, they’re convenient, but convenience isn’t everything, especially when you consider the hidden cost of reversal agents and the fact that long‑term safety data is still being collected. 😐 Plus, not every patient can afford the premium price, so warfarin remains a viable, low‑cost alternative for many. :)
Kate Marr
November 4, 2025 AT 01:27Our healthcare system should prioritize home‑grown, affordable solutions, not high‑priced imported pills pumped in by multinational conglomerates. 🇺🇸💪 The old‑school warfarin, backed by decades of data, aligns perfectly with that vision, whereas those shiny NOACs feel like a luxury import for the elite.
James Falcone
November 6, 2025 AT 22:54Warfarin's cheap price beats any NOAC any day.
Frank Diaz
November 9, 2025 AT 20:20One could argue that the relentless pursuit of newer anticoagulants reflects a deeper existential malaise: a refusal to accept the imperfect yet functional tools designed by our predecessors, opting instead for the illusion of perfection that capitalism so readily sells.
Mary Davies
November 12, 2025 AT 17:47The drama of a patient balancing blades of spinach against the ticking clock of an INR test reads like a tragic opera, each appointment a crescendo of anxiety, each result a melancholy refrain that never truly resolves.
Valerie Vanderghote
November 15, 2025 AT 15:14Let me tell you, the moment I stepped into the clinic and saw the nurse set up yet another INR lab draw, I felt like I was entering a time warp where the 20th century refused to die. The fluorescent lights flickered, the scent of antiseptic clung to the air, and the endless paperwork seemed to mock any notion of progress. Meanwhile, on the pharmacy shelf next to the warfarin bottles, the NOAC boxes gleamed with promises of “once‑daily dosing” and “no monitoring required,” like a mirage in a desert of bureaucracy. I asked the pharmacist about the cost, and the answer was a litany of numbers that could fund a small vacation. It struck me then that choosing an anticoagulant is less about medical science and more about navigating a labyrinth of financial and emotional obstacles. Patients are forced to weigh the simplicity of a pill against the uncertainty of insurance approvals, the dread of potential bleeding, and the fear of becoming a statistic in a pharmaceutical study. Yet, amidst this chaos, the human spirit persists, yearning for clarity amid the chaos. We each must decide whether we are content to follow the prescribed path of tradition or to step into the uncharted waters of newer therapy, knowing that every choice carries its own hidden currents.
Michael Dalrymple
November 18, 2025 AT 12:40It’s commendable that you’re taking the time to understand the nuances between warfarin and the newer anticoagulants. By weighing factors such as renal function, lifestyle preferences, and cost, you’re positioning yourself to make an informed decision in partnership with your clinician. Keep asking questions, and remember that shared decision‑making leads to the best outcomes.
Emily (Emma) Majerus
November 21, 2025 AT 10:07yay you’re on the right track, just keep talkin to your doc and pick what feels right for u.