Warfarin Genetics: How CYP2C9 and VKORC1 Variants Affect Bleeding Risk and Dosing
 Oct, 30 2025
Oct, 30 2025
Warfarin Dosing Calculator
Personalized Warfarin Dosing
Based on your CYP2C9 and VKORC1 genotypes
Your Recommended Starting Dose
Bleeding Risk
Why Some People Bleed Too Much on Warfarin
Warfarin has been used for over 70 years to prevent dangerous blood clots. But for many people, it’s a balancing act. Too little, and clots form. Too much, and you bleed - sometimes dangerously. About 30-40% of people on warfarin experience a serious bleeding event during treatment. That’s not random. It’s often written in their genes.
The two biggest genetic players are CYP2C9 and VKORC1. These aren’t just random letters. They’re genes that control how your body handles warfarin. If you have certain versions of these genes, your dose needs to be lower. Much lower. And if your doctor doesn’t know, you could end up in the ER with an INR of 6.2 - like one Reddit user did after being started on a standard dose.
What VKORC1 Does - And Why It Matters
VKORC1 is the actual target of warfarin. This gene makes the enzyme that recycles vitamin K, which your liver needs to make clotting factors. Warfarin blocks this enzyme. Simple enough. But not everyone’s enzyme works the same.
The most common genetic variation is at position -1639 in the VKORC1 gene. If you have two A alleles (AA), your body makes about 40% less of this enzyme than someone with two G alleles (GG). That means warfarin hits you harder. You don’t need as much of it to block what’s already low.
People with the AA genotype typically need only 5-7 mg per week of warfarin. Those with GG need 28-42 mg per week. That’s a 60-70% difference. If you’re AA and get a 5 mg daily dose - the standard starting point - your blood will thin too fast. INR spikes. Bleeding risk skyrockets.
CYP2C9: The Metabolism Switch
Warfarin comes in two forms: R and S. The S-form is five times stronger. And CYP2C9 is the enzyme that breaks it down.
Most people have the normal version: CYP2C9*1. But about 10-15% of white and Asian populations carry one or two copies of CYP2C9*2 or *3. These variants are like broken brakes. They slow down warfarin metabolism drastically.
CYP2C9*3 carriers clear S-warfarin 80% slower than normal. That means the drug builds up in their blood. Even a small dose becomes too much. In one study, patients with CYP2C9*3 had an 83% higher risk of dangerously high INR in the first week of treatment. Many report INR values over 4 - the threshold for increased bleeding risk - within days of starting.
One patient on Reddit shared: “After genetic testing revealed CYP2C9*3, my dose dropped from 5mg to 2.5mg. My INR finally stabilized after six months of rollercoaster readings.” That’s not unusual. It’s predictable.

When Both Genes Go Wrong
The real danger comes when you have bad versions of both genes. A person with VKORC1 AA and CYP2C9*3/*3 is at extreme risk.
These patients often need less than 1.5 mg per day - sometimes as low as 0.5 mg. But without testing, doctors start everyone at 5 mg. That’s like giving a child a full adult dose of insulin.
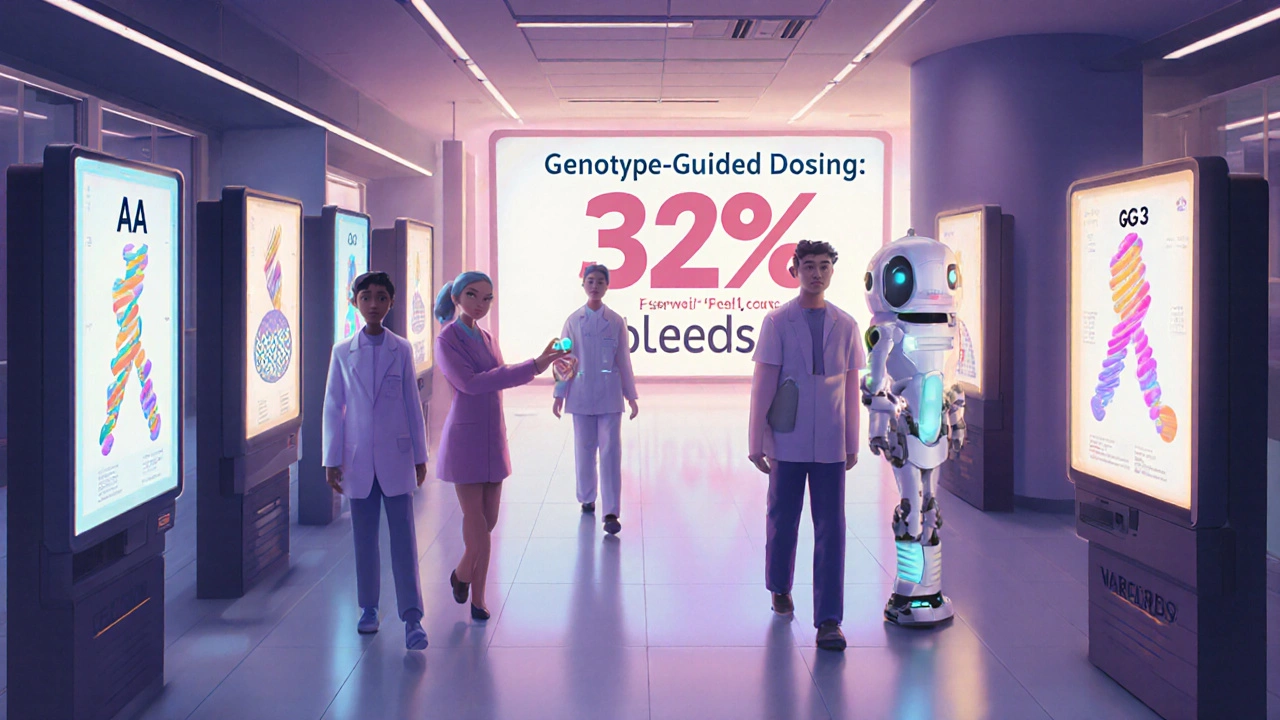
A 2020 review found that patients with this double-whammy genotype had an 83% higher risk of supratherapeutic INR in the first week. In real life, that means nosebleeds, bruising, blood in urine - or worse, brain bleeds. The EU-PACT trial showed that genotype-guided dosing cut major bleeding by 32% in the first 90 days.
Genetic Testing: What the Guidelines Say
The Clinical Pharmacogenetics Implementation Consortium (CPIC) has recommended testing since 2013. Their guidelines say: test CYP2C9 and VKORC1 before starting warfarin. Then use a simple algorithm to pick your starting dose.
But here’s the problem: only 5-15% of U.S. patients get tested. Why? Cost, confusion, and inertia.
Testing costs $250-$500 out of pocket. Medicare covers it under CPT codes 81225 and 81227. Many private insurers don’t. And many doctors - especially primary care providers - don’t know how to interpret the results. A 2023 survey found only 38% of them could correctly explain how CYP2C9*3 affects warfarin metabolism.
Still, places like Vanderbilt University Medical Center made it standard. They integrated genetic results into their electronic health records. Result? Patients reached a stable INR 1.8 days faster than those on standard dosing.
What About DOACs? Are They Better?
Direct oral anticoagulants (DOACs) like apixaban and rivaroxaban don’t need monitoring. They don’t interact with food. And they don’t depend on your genes.
That’s why their use jumped from 32% to 58% of new atrial fibrillation patients between 2010 and 2018. Warfarin use dropped by nearly a third.
But DOACs aren’t perfect. They’re expensive. They can’t be reversed easily. And they’re not safe for people with mechanical heart valves or severe kidney disease - two groups who still rely on warfarin.
For those patients, warfarin remains the only option. And for them, genetics isn’t optional. It’s essential.
Real-World Impact: Patient Stories and Data
Surveys show patients who get tested are happier. One 2022 study of 1,247 warfarin users found those with genetic testing rated their satisfaction at 7.8 out of 10. Those without testing? 6.2 out of 10.
And the clinical data backs it up. The 2025 European Heart Journal meta-analysis confirmed genotype-guided dosing reduces major bleeding by 27% in the first three months. The REAL-Gene trial in 2023 found a 8.2% improvement in time spent in the therapeutic range.
Still, some experts push back. Dr. John R. Horn argues the number needed to genotype to prevent one major bleed is 200. That sounds high. But consider this: 7.5 million Americans take warfarin every year. If even 10% of them benefit from testing, that’s 750,000 people avoiding dangerous bleeding. That’s not a small number.
What You Can Do Right Now
If you’re on warfarin and have had unstable INR readings, ask your doctor about genetic testing. If you’re about to start, ask before the first pill.
Don’t assume your dose is right because it’s “standard.” Your genes aren’t standard. Your metabolism isn’t standard. Your risk isn’t standard.
Ask if your clinic uses the CPIC dosing algorithm. If they don’t, request it. Bring the guidelines. Print them. Show them. You’re not being difficult - you’re being smart.
And if insurance denies coverage? Appeal. Cite the 2023 REAL-Gene trial. Mention CMS coverage. Point out that a single bleeding event costs the system over $30,000. Prevention is cheaper.
The Future of Warfarin
Even as DOACs rise, warfarin isn’t going away. It’s too cheap. Too reversible. Too necessary for some.
By 2030, 60% of new warfarin users are expected to get genetic testing - driven by falling test costs (projected to drop below $100 by 2027) and stronger evidence.
The Warfarin Genotype Implementation Network (WaGIN), launching in 2025, plans to enroll 50,000 patients across 200 sites. This isn’t just research. It’s scaling a solution.
Warfarin isn’t outdated. It’s misunderstood. And genetics is the key to unlocking its safety.
Do I really need genetic testing before starting warfarin?
If you’re starting warfarin for long-term use - like for atrial fibrillation, deep vein thrombosis, or a mechanical heart valve - yes. Genetic testing can prevent dangerous overdoses in the first weeks, when bleeding risk is highest. Studies show it reduces major bleeding by up to 32% in the first 90 days. Even if your doctor doesn’t offer it, ask. It’s not experimental. It’s evidence-based.
How long does genetic testing take?
Standard genetic tests for CYP2C9 and VKORC1 take about 3-5 business days. Some labs offer faster turnaround (24-48 hours) for an extra fee. The test is a simple blood draw or saliva swab. Results come back as a genotype report - for example, CYP2C9*1/*3 and VKORC1 -1639 AA. Your doctor uses that to pick your starting dose.
Is genetic testing covered by insurance?
Medicare covers CYP2C9 (CPT 81225) and VKORC1 (CPT 81227) testing for patients on warfarin. Many private insurers do too, but coverage varies. If denied, appeal using the 2023 REAL-Gene trial results or the CPIC guidelines. Some hospitals offer financial assistance or reduced-cost testing through research programs.
Can I get tested if I’m already on warfarin?
Absolutely. Even if you’ve been on warfarin for months or years, genetic testing can explain why your dose is high or low, or why your INR keeps swinging. It doesn’t change your current dose - but it helps your doctor fine-tune it. Many patients report less anxiety and fewer clinic visits after getting tested, even if they’ve been stable.
What if my doctor says genetic testing isn’t necessary?
Ask for the evidence. Cite the 2013 EU-PACT trial, the 2025 European Heart Journal meta-analysis, or the CPIC guidelines. If they’re still hesitant, ask for a referral to a hematologist or pharmacist specializing in anticoagulation. Many hospitals now have pharmacogenetics clinics. You’re not asking for a luxury - you’re asking for safer care.
Justin Vaughan
November 1, 2025 AT 05:06Matthew Kwiecinski
November 2, 2025 AT 14:05Manuel Gonzalez
November 4, 2025 AT 12:35Brittney Lopez
November 6, 2025 AT 11:14Jens Petersen
November 6, 2025 AT 18:45Keerthi Kumar
November 7, 2025 AT 22:37Dade Hughston
November 8, 2025 AT 05:42Jim Peddle
November 8, 2025 AT 20:26S Love
November 10, 2025 AT 15:41Pritesh Mehta
November 11, 2025 AT 04:25Billy Tiger
November 11, 2025 AT 23:40Katie Ring
November 13, 2025 AT 02:16Adarsha Foundation
November 14, 2025 AT 00:54Alex Sherman
November 14, 2025 AT 23:31John Concepcion
November 16, 2025 AT 19:05