Warfarin and NSAIDs: Understanding the Dangerous Bleeding Risk
 Nov, 28 2025
Nov, 28 2025
Warfarin Medication Safety Checker
When you’re on warfarin, even a simple headache can become a serious decision. Taking ibuprofen or naproxen for relief might seem harmless - but it’s not. Combining these common painkillers with warfarin doesn’t just increase your risk of bleeding. It can send you to the ER with a hemoglobin drop, internal bleeding, or worse. This isn’t a rare side effect. It’s a well-documented, life-threatening interaction that affects millions of people every year.
Why Warfarin and NSAIDs Don’t Mix
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. Without those factors, your blood takes longer to clot - that’s the point. It stops dangerous clots from forming in people with atrial fibrillation, deep vein thrombosis, or after heart valve replacements. NSAIDs - like ibuprofen, naproxen, diclofenac, and even meloxicam - work differently. They block an enzyme called COX, which reduces pain and inflammation. But that same enzyme also helps platelets stick together to form clots. So when you take an NSAID, your platelets can’t do their job properly. Put them together, and you’ve got a one-two punch: your blood can’t clot well because of warfarin, and your platelets are already weakened by the NSAID. This isn’t just additive. It’s synergistic. Studies show this combination increases the risk of bleeding by more than two times compared to warfarin alone.Which NSAIDs Are the Most Dangerous?
Not all NSAIDs are created equal when it comes to bleeding risk. Some are far worse than others. - Naproxen carries the highest risk - 4.1 times greater bleeding than warfarin alone. It’s often prescribed for arthritis, so many patients don’t realize how dangerous it is with their blood thinner. - Diclofenac isn’t far behind at 3.3 times higher risk. - Ibuprofen is commonly thought of as “safe,” but it still raises bleeding risk by 1.79 times. - Even meloxicam, often labeled as “gentler,” increases the chance of INR spikes - meaning your blood gets dangerously thin. And here’s the myth that kills people: COX-2 inhibitors like celecoxib aren’t safer. A 2020 meta-analysis confirmed they carry the same bleeding risk as traditional NSAIDs when taken with warfarin. The idea that they’re “stomach-friendly” doesn’t mean they’re blood-safe.Where Does the Bleeding Happen?
It’s not just one type of bleeding. The combination hits multiple organs: - Gastrointestinal bleeding increases by 2.24 times. This is the most common - stomach ulcers, intestinal bleeds, vomiting blood. Many patients don’t notice until they’re pale, dizzy, or passing black stools. - Intracranial bleeding (bleeding in the brain) jumps by 3.22 times. This can cause stroke-like symptoms or sudden death. - Pulmonary bleeding rises by 1.36 times - coughing up blood is a red flag. - Urinary tract bleeding increases by 1.57 times - pink or red urine isn’t normal. The FDA’s adverse event database recorded over 1,800 bleeding events linked to warfarin-NSAID use between 2015 and 2020. Over 60% of those were GI bleeds. And in 78% of cases, patients ended up hospitalized - often for over five days.What About Newer Blood Thinners?
Many patients assume switching from warfarin to a NOAC - like apixaban, rivaroxaban, or dabigatran - makes NSAIDs safe. It doesn’t. A 2019 Circulation study found that NSAIDs increase bleeding risk with all oral anticoagulants. The ARISTOTLE trial showed apixaban might be slightly safer than warfarin when NSAIDs are used, but the risk is still significantly elevated. And a 2020 study found dabigatran had lower bleeding risk than warfarin with NSAIDs - but rivaroxaban was just as risky. The bottom line: no oral anticoagulant is safe with NSAIDs. Even if your doctor switched you to a “newer” blood thinner, that doesn’t mean you can take ibuprofen for back pain.
Real People, Real Consequences
Reddit threads, patient forums, and medical journals all tell the same story: > “I took two ibuprofen for a headache. My INR jumped from 2.8 to 6.1 in 48 hours. I ended up in the ER with a hemoglobin drop from 14 to 8. I lost a unit of blood.” - Reddit user, March 2023 > “I didn’t tell my doctor I was taking Advil for my knees. I started passing dark blood. They found a bleeding ulcer. I was in the hospital for a week.” - PatientsLikeMe, 2022 On Drugs.com, over 1,400 reviews of warfarin-NSAID combinations have an average safety rating of 2.1 out of 10. Eighty-seven percent of those reviews say: “Don’t do this.” These aren’t outliers. They’re predictable outcomes of a well-known interaction.What Should You Do Instead?
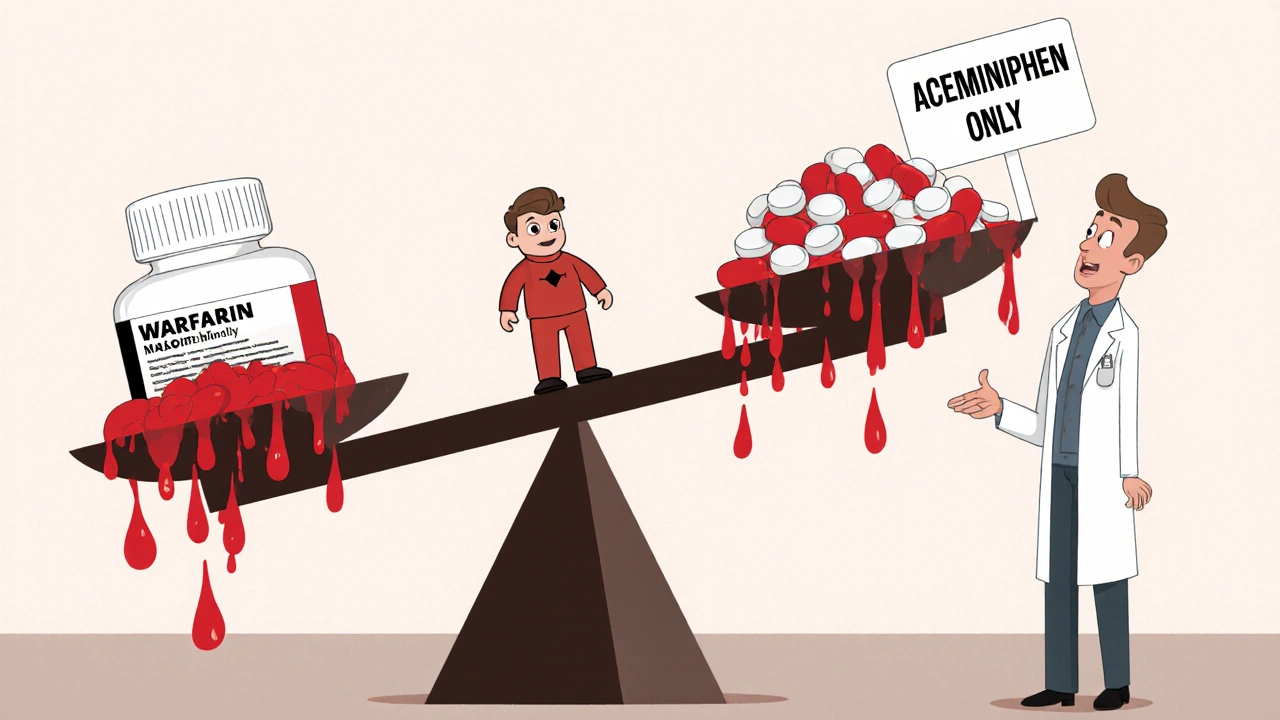
The safest alternative? Acetaminophen (Tylenol). It doesn’t affect platelets or the stomach lining. Studies show it’s the go-to pain reliever for warfarin users - used by over 23% of them as a substitute. Other options: - Topical pain relievers - gels or patches with menthol, capsaicin, or lidocaine. They’re absorbed through the skin, not the bloodstream. Sales in this group are growing 12.7% annually among anticoagulant users. - Physical therapy - for chronic joint or back pain. It reduces reliance on pills entirely. - Cold or heat therapy - simple, free, and effective for muscle aches. - Low-dose aspirin - only if prescribed. It’s an NSAID too, but sometimes used for heart protection. Never take it without your doctor’s approval. If you’re still in pain and acetaminophen isn’t enough, talk to your doctor about non-drug options or short-term alternatives - not a quick fix from the pharmacy.What If You’ve Already Taken an NSAID?
If you accidentally took an NSAID - even one dose - here’s what to do:- Call your anticoagulation clinic or doctor immediately.
- Get your INR checked within 24-72 hours.
- Watch for signs of bleeding: unusual bruising, nosebleeds, dark stools, pink urine, headaches, dizziness, or vomiting blood.
- Don’t wait for symptoms. Bleeding can start quietly.
Why Do Doctors Still Prescribe This?
It’s frustrating, but it happens. Here’s why: - Patient non-disclosure: 68% of warfarin-related bleeding cases involve patients who didn’t tell their doctor they were taking over-the-counter NSAIDs. They think “it’s just Advil.” - Electronic health records: 42% of U.S. hospitals still don’t flag this dangerous combo automatically. - Outdated labels: Many NSAID packages only say “may increase bleeding risk” - they don’t mention warfarin specifically. - Prescription habits: Doctors treating arthritis or back pain may not realize how high the risk is - especially if they’re not trained in anticoagulation. The Anticoagulation Forum’s 2022 guidelines are clear: if NSAIDs are unavoidable, use the lowest dose for the shortest time, avoid naproxen and meloxicam, check INR before and after, and give patients a proton pump inhibitor to protect the stomach. But even that’s not ideal. The Institute for Safe Medication Practices rates this combination as “high risk with no acceptable safe use parameters.”The Bigger Picture
About 3.1 million Americans take warfarin. Over 17 million use NSAIDs monthly. That means millions are at risk. The cost? Over $1.8 billion a year in hospital bills, ER visits, and lost work. The good news? Between 2015 and 2022, warfarin-NSAID co-prescribing dropped by 27%. Why? More people switched to NOACs. But here’s the twist: NSAID use with NOACs increased by 35%. That’s because patients and even some doctors think NOACs are safe with painkillers. They’re not. The 2024 American College of Chest Physicians guidelines will make this even clearer: avoid all NSAIDs with all oral anticoagulants. Especially if you’re over 75 - your bleeding risk triples.Final Takeaway
This isn’t about being overly cautious. It’s about survival. Warfarin and NSAIDs together are a dangerous mix - no exceptions, no safe doses, no exceptions for “just one pill.” If you’re on a blood thinner:- Never take an NSAID without talking to your doctor.
- Always check the label of every OTC medicine - many cold, flu, and headache pills contain NSAIDs.
- Use acetaminophen instead - it’s the standard for a reason.
- If you’ve taken an NSAID, get your INR checked right away.
Phil Thornton
November 30, 2025 AT 10:59This is the kind of post that makes you stop scrolling and actually think.
Barbara McClelland
November 30, 2025 AT 22:21I’m a nurse and I see this every single week. Someone comes in with a bleeding ulcer because they took Advil for their arthritis and didn’t think it mattered. Please, if you’re on warfarin, treat NSAIDs like poison. Acetaminophen is your friend.
Ady Young
December 1, 2025 AT 06:02My grandma was on warfarin for AFib and her doctor never warned her about OTC meds. She ended up in the hospital after a week of taking ibuprofen for her knees. We didn’t even know it was a problem until her INR was through the roof. This post saved my life - I’m now double-checking every label on every bottle in our medicine cabinet.
Daniel Rod
December 2, 2025 AT 12:16It’s wild how medicine keeps repeating the same mistakes. We have decades of data on this interaction, yet people still think ‘it’s just one pill.’ The real tragedy isn’t the bleeding - it’s that this could be prevented with better education. Not just for patients, but for doctors too. If your GP doesn’t know this, they shouldn’t be prescribing anticoagulants.
I’ve seen people switch to NOACs thinking they’re free passes to pop NSAIDs. Nope. Same risk. Same consequences. The system is broken when the safest option is acetaminophen - a drug that’s been around since the 1800s.
We need better labeling. Better alerts. Better training. And we need to stop treating patients like they’re supposed to know all the hidden dangers in every pill bottle.
Also - topicals. They’re underused. A capsaicin patch costs less than a bottle of ibuprofen and doesn’t touch your blood. Why isn’t this the first recommendation?
And yes, I’m that guy who reads the FDA’s adverse event database for fun. This combo is a horror story waiting to happen.
Clay Johnson
December 4, 2025 AT 09:44The paradox of modern medicine: we have more data than ever, yet less wisdom in practice.
Warfarin isn’t the villain. NSAIDs aren’t evil. The system is. The lack of interoperability between EHRs, the silence of pharmacy interfaces, the assumption that patients will read labels - these are failures of design, not negligence.
And yet we blame the patient. We blame the doctor. We blame the pharmacist.
The real culprit is the illusion of safety. A pill is small. A label is small. A warning is small. But the consequence? It’s not small.
There is no such thing as a ‘safe’ dose when two mechanisms converge to disable your body’s last line of defense.
We don’t need more studies. We need mandatory alerts. We need standardized language. We need to treat this like a nuclear reactor, not a headache.
And if you’re still using naproxen? Stop. Now.
It’s not about being careful. It’s about being alive.
Ifeoma Ezeokoli
December 5, 2025 AT 16:07I’m from Nigeria and we don’t have the same access to NOACs, but we know this danger. My cousin took diclofenac for back pain and bled out at home. No ER. No lab. Just a body on the floor. This isn’t an American problem. It’s a human problem. And no one is listening.
Travis Freeman
December 6, 2025 AT 05:47My dad is 82 and on warfarin. He still takes Aleve because he says ‘it’s what he’s always done.’ I printed out this entire post and taped it to his medicine cabinet. He hasn’t touched an NSAID since. Sometimes, the only thing that works is a printed-out truth.
Astro Service
December 6, 2025 AT 13:55Big Pharma doesn’t want you to know this. Why? Because acetaminophen doesn’t make them billions. NSAIDs? They’re everywhere. That’s why the labels are vague. That’s why your doctor doesn’t warn you. It’s all about profit.
And now they’re pushing NOACs like magic pills. Same problem. Different price tag.
Trust no one. Check every label. Always.
DENIS GOLD
December 7, 2025 AT 05:26Why are we even having this conversation? If you’re dumb enough to mix warfarin with NSAIDs, you deserve what you get. Stop being a liability to the healthcare system.
farhiya jama
December 8, 2025 AT 05:47I took naproxen for a week and didn’t realize my INR was sky-high until I was vomiting blood. I’m lucky I didn’t die. Now I only use Tylenol. And I hate it. But I’m alive. So yeah. Worth it.
Evelyn Salazar Garcia
December 8, 2025 AT 09:12Why is this even a thing? Just ban NSAIDs for people on blood thinners. Problem solved.
Alexander Levin
December 8, 2025 AT 23:15They’re all lying. The FDA knows NSAIDs are deadly with warfarin. They just don’t care. 1.8 billion in hospital bills? That’s just profit to them. 😈