Molnupiravir vs Paxlovid and Other COVID‑19 Antivirals: A Detailed Comparison
 Oct, 10 2025
Oct, 10 2025
COVID-19 Antiviral Comparison Tool
Recommended Treatment
Molnupiravir
Efficacy: ~30% reduction in hospitalization
Form: Oral capsule
Cost: £200 (UK)
Safety: Mild side effects; theoretical mutagenicity concerns
Paxlovid
Efficacy: ~89% reduction in hospitalization
Form: Oral tablets
Cost: Free (UK NHS)
Safety: Drug interactions, altered taste
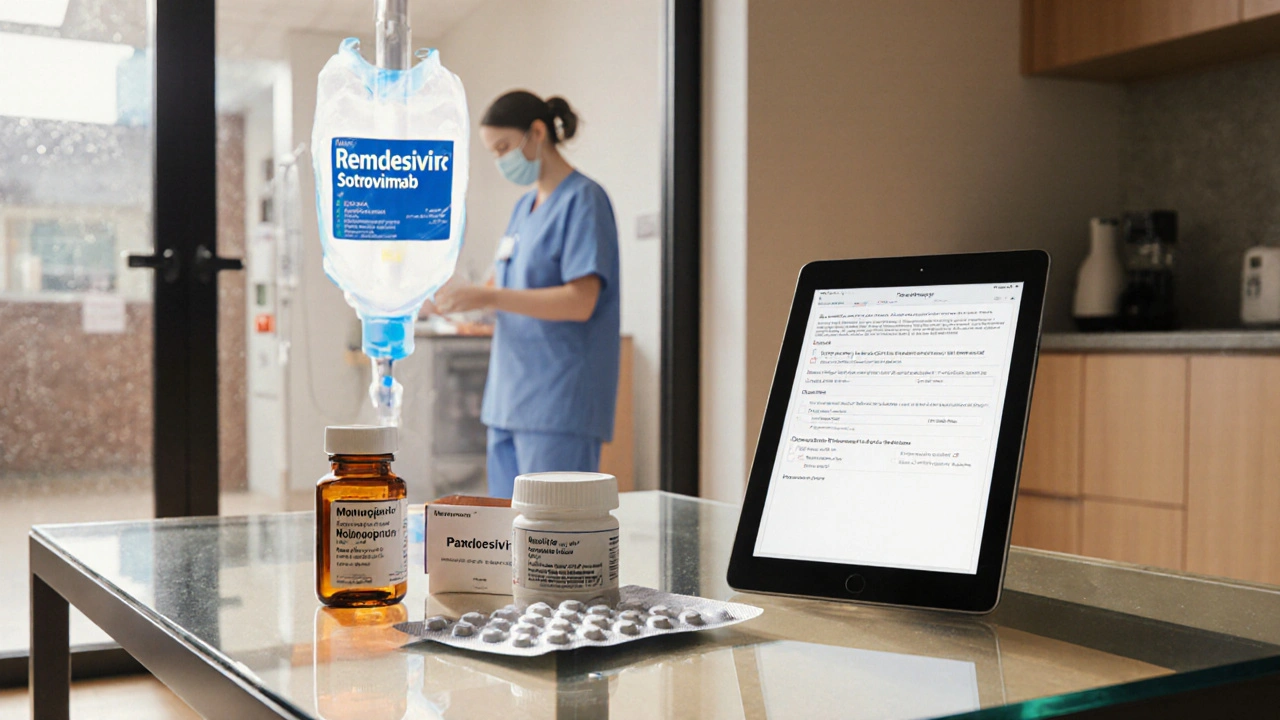
Remdesivir
Efficacy: ~87% reduction in severe disease
Form: IV infusion
Cost: £3,000 (UK)
Safety: Liver/kidney issues, infusion site reactions
Sotrovimab
Efficacy: ~85% reduction in hospitalization
Form: IV infusion
Cost: Not specified
Safety: Infusion-related reactions
Key Takeaways
- Molnupiravir is taken as a simple oral capsule, but its efficacy (≈30% reduction in hospitalisation) is lower than Paxlovid’s ≈89%.
- Paxlovid (nirmatrelvir/ritonavir) needs a food‑level dosing schedule and has drug‑interaction warnings.
- Remdesivir is an IV drug, best for hospital settings, with a 5‑day course showing roughly 87% effectiveness in early use.
- Cost and availability vary: Molnupiravir is cheapest in the UK NHS formulary, Paxlovid is subsidised in the US, while Remdesivir remains expensive and limited to hospitals.
- Safety profiles differ: Molnupiravir’s main concern is mutagenic potential (still under review), Paxlovid can affect liver enzymes, Remdesivir may raise liver enzymes and cause kidney issues.
What Is Molnupiravir?
When treating COVID‑19 at home, Molnupiravir is a synthetic nucleoside analogue that forces the virus to make copying errors, leading to a non‑viable virus. The drug was originally developed for influenza, then repurposed for SARS‑CoV‑2 during the pandemic. It comes in 200mg capsules taken twice daily for five days, ideally within five days of symptom onset.
Major Alternatives at a Glance
Three antivirals dominate the outpatient landscape:
- Paxlovid - a combination of nirmatrelvir (protease inhibitor) and ritonavir (pharmacokinetic booster). Taken as two 150mg tablets of nirmatrelvir plus one 100mg tablet of ritonavir, twice daily for five days.
- Remdesivir - an intravenous nucleotide analogue administered once daily for three days (early use) or five days (hospitalised patients).
- Sotrovimab - a monoclonal antibody given as a single IV infusion; works by neutralising the spike protein.
Efficacy Benchmarks from Clinical Trials
Understanding the numbers helps you decide which drug matches your risk profile.
| Drug | Study Population | Relative Risk Reduction | Key Findings |
|---|---|---|---|
| Molnupiravir | Unvaccinated adults, median age 45 | ≈30% | Reduced hospitalisation from 9.7% to 6.8% in the MOVe‑OUT trial (2021). |
| Paxlovid | High‑risk adults, median age 56 | ≈89% | EPIC‑HR trial showed hospitalisation drop from 6.3% to 0.8%. |
| Remdesivir | Outpatients within 7days of symptoms, median age 50 | ≈87% | ACT‑1 trial reported 87% reduction in progression to severe disease. |
| Sotrovimab | Adults ≥18y, high‑risk, median age 58 | ≈85% | COMET‑ICE study: 85% lower risk of hospitalisation. |
Numbers differ because trial designs, variants, and vaccination status influence outcomes. In a fully vaccinated population, absolute benefits shrink, but Paxlovid still leads the pack.
Safety and Side‑Effect Profiles
All drugs carry risks; weighing them against benefits is essential.
- Molnupiravir: Generally well‑tolerated; most common complaints are mild nausea and diarrhoea. Theoretical mutagenicity raised concerns, but regulatory reviews (FDA, EMA) have deemed the risk low for short courses.
- Paxlovid: Ritonavir inhibits CYP3A4, so many drugs (statins, anti‑arrhythmics, certain anti‑seizure meds) need dose adjustments. Side effects include altered taste, diarrhoea, and rare liver enzyme spikes.
- Remdesivir: Requires IV access; can cause elevated liver enzymes, renal dysfunction, and infusion‑site reactions.
- Sotrovimab: Mostly infusion‑related - mild fever, headache, rare allergic reactions.

Cost, Accessibility, and Regulatory Status (2025)
Availability differs across regions. Here’s a quick snapshot for the UK, US, and EU.
- UK (NHS): Molnupiravir is listed on the NHS Formulary at £200 per course; Paxlovid is provided free under the NHS COVID‑19 Antiviral Programme; Remdesivir is hospital‑only, costing around £3,000 per five‑day course.
- US: Paxlovid is covered by most insurers and by the government’s Treatment Access Program; Molnupiravir is priced at $700 per course; Remdesivir is reimbursed for inpatient use at roughly $5,000.
- EU: Molnupiravir received EMA conditional approval in 2022, with price negotiations ongoing; Paxlovid is approved across the bloc and often included in national reimbursement schemes.
Practical Decision Guide
Use the following flow to pick the right antiviral:
- Confirm COVID‑19 diagnosis and symptom onset <5days ago.
- Assess risk factors (age>65, immunocompromised, obesity, diabetes, cardiovascular disease).
- If high‑risk and no contraindications to ritonavir, Paxlovid is the first‑line choice.
- If Paxlovid is unavailable or patient takes interacting meds that cannot be paused, consider Molnupiravir (provided the patient is not pregnant).
- For patients already hospitalised or requiring IV therapy, Remdesivir becomes appropriate.
- When monoclonal antibodies are still effective against circulating variants, Sotrovimab offers an alternative.
Always discuss with a healthcare professional, especially if you have liver or kidney disease.
Frequently Asked Questions
Can I take Molnupiravir if I’m pregnant?
Current guidance advises against using Molnupiravir during pregnancy because animal studies showed potential fetal harm. Pregnant patients should be offered Paxlovid (if no contraindications) or monoclonal antibodies.
How quickly does Paxlovid start working?
Viral load reduction is seen within 24‑48hours of the first dose, aligning with the drug’s rapid protease inhibition.
Do I need a prescription for these antivirals?
Yes. All four treatments (Molnupiravir, Paxlovid, Remdesivir, Sotrovimab) require a prescription from a qualified clinician. In many countries, high‑risk patients can receive a same‑day prescription through telehealth services.
Is there a difference in efficacy against Omicron sub‑variants?
Paxlovid retains activity across all Omicron sub‑variants because it targets a conserved viral protease. Molnupiravir’s mechanism (error‑inducing replication) also works, but real‑world data show a modest dip in effectiveness for newer lineages.
Can I take Molnupiravir and a COVID‑19 vaccine booster together?
Yes. The antiviral does not interfere with the immune response to the vaccine. However, the booster should be administered before infection, as antivirals treat an existing infection rather than prevent it.
Eric Appiah Tano
October 10, 2025 AT 18:39Great rundown of the antivirals, especially the clear breakdown of efficacy vs. cost. For someone on the fence, the practical decision guide really helps translate the data into everyday choices. I appreciate the note on drug interactions with Paxlovid – that’s a common snag for many patients on statins. The inclusion of regional pricing makes it easier to see what’s actually affordable. Overall, a solid resource for both clinicians and the general public.
Jonathan Lindsey
October 11, 2025 AT 18:16One must commend the author for assembling a comprehensive tableau that juxtaposes pharmacodynamic potency, pharmacokinetic convenience, and fiscal ramifications across a spectrum of therapeutic agents. The discourse initiates with an elucidation of Molnupiravir’s mechanistic propensity to induce mutagenesis, a nuance often eclipsed by headline efficacy percentages. Subsequently, the treatise expounds upon Paxlovid’s protease inhibition, underscoring its remarkable 89% relative risk reduction while cautioning about CYP3A4-mediated drug interactions. The manuscript proceeds to delineate Remdesivir’s intravenous administration logistics, contextualizing its high cost within hospital infrastructure constraints. Moreover, the exposition astutely references Sotrovimab’s monoclonal antibody architecture, noting its attenuated efficacy against emergent sub‑variants. The integration of regional cost analyses for the UK, US, and EU endows the reader with a pragmatic appreciation of health‑economic disparities. Notably, the safety profile segment juxtaposes mild gastro‑intestinal disturbances associated with Molnupiravir against the taste alteration phenomenon observed with Paxlovid. The author further incorporates a decision algorithmic flowchart, facilitating actionable clinical pathways for diverse risk cohorts. While the treatise excels in breadth, a deeper exploration of real‑world effectiveness amid vaccinated populations would enrich the discourse. Nonetheless, the synthesis of trial data, regulatory status, and practical guidance culminates in an invaluable compendium for stakeholders traversing the antiviral landscape.
Gary Giang
October 12, 2025 AT 17:53Interesting analysis; the color‑coded efficacy chart really paints a vivid picture of the trade‑offs. I’m particularly drawn to the way the author frames Molnupiravir as the "budget-friendly" option, even though the efficacy gap remains sizable. The reserved tone underscores the uncertainty surrounding mutagenicity, which feels appropriate given the data. Overall, a balanced piece that respects both scientific rigor and layperson readability.
steve wowiling
October 13, 2025 AT 17:29Wow, drama in a pill.
Warren Workman
October 14, 2025 AT 17:06While the author paints a rosy picture of Paxlovid’s 89% efficacy, let’s not forget the hidden pharmacokinetic labyrinth imposed by ritonavir’s CYP3A4 inhibition. The cost‑benefit matrix is further muddied when you consider real‑world adherence challenges and the potential for off‑label polypharmacy clashes. In other words, the “first‑line” label feels more like a marketing spin than an unequivocal clinical mandate.
king singh
October 15, 2025 AT 16:43Appreciate the nuanced view; note that for patients on statins, a temporary pause may mitigate interaction risks without sacrificing overall benefit.
Adam Martin
October 16, 2025 AT 16:19Reading through this, I’m reminded how crucial it is to tailor antiviral choice to the individual’s comorbidity profile. Paxlovid’s protease blockade shines for high‑risk patients, yet the drug‑interaction hurdle can be a show‑stopper for those on complex regimens. Molnupiravir, though modest in efficacy, offers a safe harbor for patients who can’t tolerate ritonavir or lack IV access. Remdesivir remains the hospital‑centric stalwart, but its cost barrier is non‑trivial. Meanwhile, Sotrovimab’s utility is waning as new variants emerge, though it still has a niche for immunocompromised hosts. The decision tree the author provides is a helpful scaffold, but clinicians must also weigh vaccine‑derived immunity, which can tilt the absolute benefit curve dramatically. All in all, a solid primer that balances data and practical guidance.
Ryan Torres
October 17, 2025 AT 15:56All this "clinical data" sounds convincing until you realize the pharma giants are pulling the strings behind the scenes 😠💊. Don’t be fooled by the fancy percentages; the real agenda is profit, not patient health.
shashi Shekhar
October 18, 2025 AT 15:33Ah, the classic conspiracy cocktail-mix a dash of “profit motive” with a splash of “hidden side‑effects,” and you’ve got a perfect recipe for viral posts. Let’s not forget the irony of questioning data while ignoring the peer‑review process.
Marcia Bailey
October 19, 2025 AT 15:09Excellent summary! The clear tables make it easy to compare, and the inclusion of real‑world cost data is super helpful 😊. Thanks for putting this together.
Hannah Tran
October 20, 2025 AT 14:46Very friendly write‑up, but let’s cut the fluff-Paxlovid is still the MVP for high‑risk folks, and any talk of “alternative” should come with a strong disclaimer about efficacy drop.
Dhananjay Sampath
October 21, 2025 AT 14:23Great job; however, I would like to point out that the efficacy percentages cited are relative risk reductions; absolute risk reductions may be considerably lower, especially in vaccinated populations.
kunal ember
October 22, 2025 AT 13:59The article does a commendable job of summarizing the current antiviral landscape; however, for readers who wish to delve deeper into the pharmacological underpinnings, it would be beneficial to elaborate on the mechanistic distinctions between nucleoside analogues such as Molnupiravir and protease inhibitors like Paxlovid. In particular, an exploration of how error‑inducing mutagenesis differs from protease blockade could illuminate why resistance patterns may evolve under selective pressure. Moreover, the piece could benefit from a brief discussion on the impact of viral variant evolution on the neutralization capacity of monoclonal antibodies, especially Sotrovimab. Finally, providing a concise overview of the regulatory pathways that led to conditional approvals versus full approvals would enhance readers' appreciation of the risk–benefit calculus employed by agencies.