Medication Dosage Adjustments for Aging Bodies and Organs
 Jan, 9 2026
Jan, 9 2026
When you’re 75, your body doesn’t process medicine the way it did at 45. That’s not just a guess-it’s science. Every organ changes with age, and those changes directly affect how drugs work in your system. A pill that helped you sleep at 60 might leave you dizzy at 80. A blood pressure med that kept your numbers steady could send your heart racing if the dose hasn’t been adjusted. This isn’t about being frail or weak. It’s about physiology. And ignoring it puts older adults at serious risk.
Why Aging Changes How Drugs Work
Your body’s ability to absorb, distribute, metabolize, and get rid of drugs all slow down as you age. It’s not one thing-it’s four systems working together that shift over time.Stomach acid drops by 20-30%, so some pills don’t dissolve as well. Blood flow to the intestines slows, meaning less medicine gets into your bloodstream. Your body fat increases by 15-20%, while muscle mass drops by 10-15%. That means drugs that like fat-like some antidepressants or sedatives-stick around longer. Drugs that need muscle to move around? They don’t reach their target as easily.
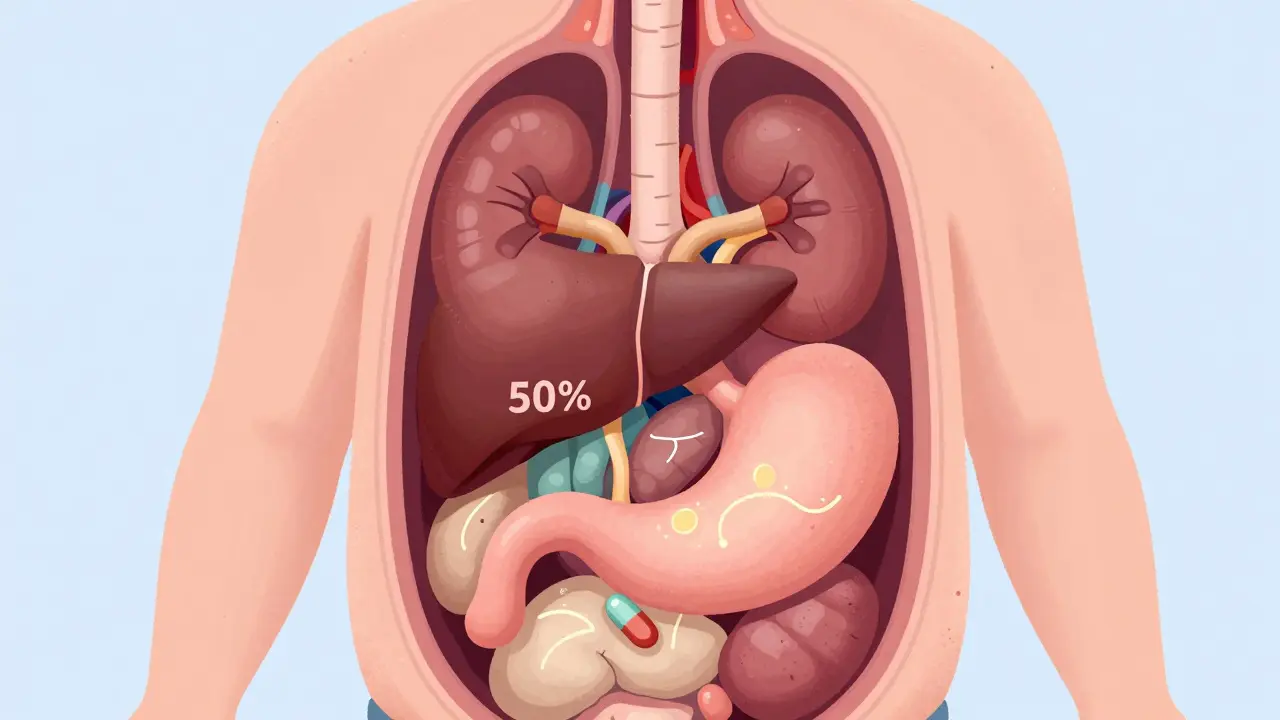
Your liver, which breaks down most medications, loses up to half its efficiency after 65. And your kidneys? They’re the biggest concern. After age 30, kidney function drops about 8 mL per minute every decade. By 70, nearly 40% of people have kidney function low enough to require a dose change. That’s not rare-it’s normal.
That’s why a standard dose of gabapentin for nerve pain (300 mg) might be too much for someone over 70. The right starting dose? 100-150 mg. Too high, and you risk falls, confusion, or hospitalization.
The ‘Start Low, Go Slow’ Rule
This isn’t just a slogan. It’s the gold standard in geriatric medicine, backed by decades of research from the American Geriatrics Society and the FDA. The idea is simple: begin with the smallest possible dose, then wait. Watch. Adjust.For example, metformin-a common diabetes drug-is usually started at 500 mg daily in younger adults. But for seniors, especially those with even mild kidney issues, doctors start at 250 mg and increase only if blood sugar stays high after 4-6 weeks. If kidney function (eGFR) drops below 45, the dose is cut again. Below 30? It’s stopped entirely.
The same goes for blood thinners like warfarin. Older adults often need 20-30% less than younger patients. Too much? Risk of internal bleeding. Too little? Risk of stroke. Finding the balance takes time, patience, and regular blood tests.
Even common painkillers like ibuprofen or naproxen become dangerous. They raise the risk of stomach bleeding by 300% in seniors. Acetaminophen is safer, but even that can harm the liver if taken daily over time. For many older adults, non-drug options-heat, physical therapy, braces-are better first steps.
How Doctors Calculate the Right Dose
It’s not guesswork. There are formulas doctors use to estimate how well your kidneys are working. The most common one is the Cockcroft-Gault equation. It takes your age, weight, and a simple blood test for creatinine.Here’s the formula: CrCl = [(140 - age) × weight in kg] / [72 × serum creatinine] (multiply by 0.85 if you’re female).
If your result is below 50 mL/min, most drugs cleared by the kidneys need a dose reduction. That includes antibiotics, diuretics, and many heart medications.
For drugs processed by the liver-like some antidepressants or pain meds-doctors check liver function with blood tests and sometimes use the Child-Pugh score. A score of 7-9 means 50% dose reduction. A score of 10 or higher? The drug might need to be avoided entirely.
But here’s the problem: only 15% of common medications have clear, easy-to-use dosing rules for seniors. For the rest, doctors rely on experience, caution, and close monitoring.
High-Risk Medications You Should Know
The 2023 Beers Criteria® lists 30 classes of drugs that are risky for older adults. These aren’t obscure pills-they’re widely prescribed.- Benzodiazepines (like lorazepam or diazepam): Increase fall risk by 50%. Can cause confusion and memory loss. Often prescribed for anxiety or sleep-but rarely safe long-term.
- Anticholinergics (like diphenhydramine, oxybutynin): Found in many sleep aids, allergy meds, and bladder pills. Double dementia risk with long-term use.
- NSAIDs (ibuprofen, naproxen): As mentioned, 300% higher risk of stomach bleeding. Even occasional use can be dangerous.
- Antipsychotics (used off-label for agitation): Increase stroke and death risk in dementia patients. Not a first-line treatment.
- Insulin and sulfonylureas (for diabetes): Too much can cause dangerous low blood sugar, leading to falls or seizures.
These aren’t banned. But they should be used only when absolutely necessary-and at the lowest possible dose for the shortest time.
What You Can Do: The Brown Bag Review
The biggest problem isn’t what doctors prescribe-it’s what patients take. Most seniors take 5 or more medications. Some are over-the-counter. Some are supplements. Some are leftovers from old conditions.Bring everything you take to your next doctor visit. Pill bottles, patches, vitamins, herbal teas-everything. This is called the “brown bag review.” It’s simple. It’s free. And it prevents errors.
One study found that when pharmacists did this review, medication errors dropped by 67%. They found duplicate drugs, expired pills, dangerous combinations. One man was taking four different pills for the same condition. Another was on a blood thinner and an NSAID together-deadly combo.
Ask your pharmacist: “Is this still right for me?” Don’t assume it is. Your body changes. Your needs change. Your meds should too.

When to Ask for Help
You don’t have to figure this out alone. Clinical pharmacists who specialize in geriatrics are your best ally. They’re trained to untangle complex drug regimens. Many hospitals and clinics now have them on staff-up from 41% in 2015 to 73% in 2023.Ask your doctor: “Can you refer me to a geriatric pharmacist?” Or call your local pharmacy. Many offer free medication reviews.
If you or a loved one has started falling more, feeling confused, losing appetite, or having strange mood swings-don’t blame it on aging. Ask: “Could this be the medicine?”
Some medications take weeks to show side effects. That’s why regular check-ins matter. Every 3-6 months, review your list. If you’ve been on a drug for over a year without a clear reason, ask if you still need it.
The Future of Senior Medication Safety
The FDA now requires drug trials to include more older adults. In 2010, only 28% of participants were over 65. By 2022, that jumped to 42%. It’s still not enough-but it’s moving.New tools are emerging. AI algorithms can now predict the right dose based on kidney function, weight, age, and other meds. One pilot at Johns Hopkins cut dosing errors by 47%.
The next big shift? Moving from “chronological age” to “functional age.” A 75-year-old who walks fast, thinks clearly, and lives independently might need the same dose as a 60-year-old. A 70-year-old who struggles to stand up or remembers names poorly? They need lower doses-even if their blood tests look fine.
This isn’t science fiction. It’s the future of care. And it’s already happening in places that prioritize safety over speed.
Final Thought: Medication Isn’t a Set It and Forget It
You wouldn’t drive a car without checking the oil. Yet many people take pills the same way-year after year, without review.Medication for seniors isn’t about taking more. It’s about taking less. Taking smarter. Taking only what’s truly needed.
Your body isn’t broken. It’s changed. And your medicines should change with it.
Jay Amparo
January 10, 2026 AT 01:56Man, this hit home. My dad was on five meds before his pharmacist caught he was taking two different versions of the same blood thinner. One was expired. The other was prescribed by a different doctor who didn’t know about the first. He nearly bled out in the kitchen. Now he only takes three-and he’s got more energy than I do.
It’s not about cutting pills-it’s about cutting clutter. Your body’s not broken, it’s just… rewired. And yeah, the brown bag review? Do it. Bring the whole damn kitchen sink. I did. My grandma’s aloe vera gel turned out to be full of NSAIDs. Who knew?
Lisa Cozad
January 11, 2026 AT 12:06I’m a nurse in a geriatric unit, and I see this every single day. One woman came in with confusion and falls-turned out she was taking Benadryl for sleep every night. For ten years. No one ever asked. She didn’t even know it was an anticholinergic. We swapped it for melatonin and light therapy. Within a week, she was telling jokes again.
Doctors don’t always know. Pharmacists? They’re the real heroes here. Ask for a med review. Don’t wait for a crisis. Your grandma’s ‘little sleep pill’ could be stealing her memory.
Saumya Roy Chaudhuri
January 12, 2026 AT 06:51Ugh, this is so basic. If you didn’t know that kidney function declines with age, you’ve been living under a rock. The Cockcroft-Gault equation? Every med student learns it in Year 1. And the Beers Criteria? It’s been around since 1991. Why are we treating this like some groundbreaking revelation?
Also, acetaminophen isn’t ‘safer’-it’s just less likely to bleed you out. But liver toxicity? Oh yeah. 4,000 mg/day is the limit. Most seniors take 1,500 mg three times a day and call it ‘natural pain relief.’ Spoiler: it’s not. Your liver doesn’t care if you call it ‘herbal’ or ‘holistic.’
Ritwik Bose
January 14, 2026 AT 03:23Thank you for this thoughtful and meticulously researched piece. 🙏 It is with profound respect for the dignity of aging individuals that I commend the emphasis on functional age over chronological age. The integration of AI-driven dosing algorithms, as referenced from Johns Hopkins, represents a paradigm shift toward precision geriatric pharmacotherapy.
May I respectfully suggest that future iterations include a brief glossary of clinical terms (e.g., eGFR, CrCl, Child-Pugh) for lay readers? Such an addition would enhance accessibility without diluting the scientific rigor. Truly commendable work.
Paul Bear
January 15, 2026 AT 11:04Let’s be clear: this isn’t ‘medicine for seniors.’ This is medicine that respects human physiology. The fact that we even have to write articles like this is a failure of medical education.
Doctors are still prescribing benzodiazepines to 80-year-olds like they’re treating anxiety, not iatrogenic dementia. NSAIDs? Still handed out like candy. And don’t get me started on the 30% of seniors on statins with no primary prevention indication.
The ‘start low, go slow’ rule isn’t a suggestion-it’s a minimum standard. If your prescriber doesn’t know Cockcroft-Gault by heart, find a new doctor. Your life isn’t a trial run.
lisa Bajram
January 17, 2026 AT 10:48OMG YES!! I’m a 68-year-old yoga instructor and I’ve been on gabapentin for neuropathy since 2018. My pharmacist said, ‘Honey, you’re taking 300 mg three times a day. That’s a 900 mg dose. You’re 68. Your kidneys are doing their best. Try 100 mg once a day.’ I did. I didn’t fall. I didn’t feel foggy. I still sleep better.
And my herbal tea? Turns out the ‘nerve calm’ blend had valerian root-anticholinergic. I tossed it. Now I just do breathing exercises. And I feel more alive than I have in years.
Bring your brown bag. Talk to your pharmacist. They’re not just the pill people-they’re your lifeline. 💪🌿
Jaqueline santos bau
January 18, 2026 AT 01:40I hate to say it, but this whole post feels like a guilt trip for older people. ‘Oh, you’re old, so you can’t take medicine like a normal person.’ What’s next? ‘You’re 75, so you shouldn’t walk up stairs.’
My aunt is 82, takes 8 meds, and still hikes every weekend. She’s got a better gait than my 30-year-old nephew. Maybe her body’s just better adapted? Maybe the ‘rules’ don’t apply to everyone?
Also, why is everyone so obsessed with ‘dose reduction’? Why not fix the kidneys instead of just lowering the pill?
Just saying-aging isn’t a disease. Don’t treat it like one.
Aurora Memo
January 20, 2026 AT 01:18Thank you for writing this with such care. I’ve seen too many elderly patients dismissed as ‘just getting old’ when the real issue was a toxic med cocktail.
One thing I’d add: don’t be afraid to say ‘I don’t want this anymore.’ You have the right to refuse any medication-even if it was prescribed by a doctor. Your body, your choice.
And if your doctor rolls their eyes when you ask about deprescribing? Find a new one. There are so many great geriatricians and pharmacists out there who want to help, not just prescribe.
Faith Edwards
January 21, 2026 AT 21:10How quaint. A 2,000-word essay on what every pharmacologist learned in med school. The Beers Criteria? Cockcroft-Gault? The fact that you felt the need to explain these to a general audience speaks volumes about the state of public health literacy.
And yet, you still missed the elephant in the room: polypharmacy is not a physiological inevitability-it’s a systemic failure of healthcare fragmentation. Three doctors. Two specialists. Five pharmacies. One confused patient.
Fix the system. Don’t just tell seniors to bring their brown bags. Fix the incentives that reward prescribing over deprescribing. Fix the insurance models that pay for pills, not reviews.
This article is a Band-Aid on a hemorrhage.