Immunotherapy for Allergies: Allergy Shots vs. Sublingual Tablets Explained
 Dec, 16 2025
Dec, 16 2025
If you’ve spent years sneezing through spring, coughing from dust mites, or panicking after a bee sting, you know that antihistamines only give you temporary relief. What if you could actually change how your body reacts to allergens - not just mask the symptoms? That’s what immunotherapy does. It’s not a quick fix. It’s a long-term plan that retrains your immune system to stop overreacting to things like pollen, dust, or pet dander. And for many people, it’s the only treatment that offers real, lasting relief.
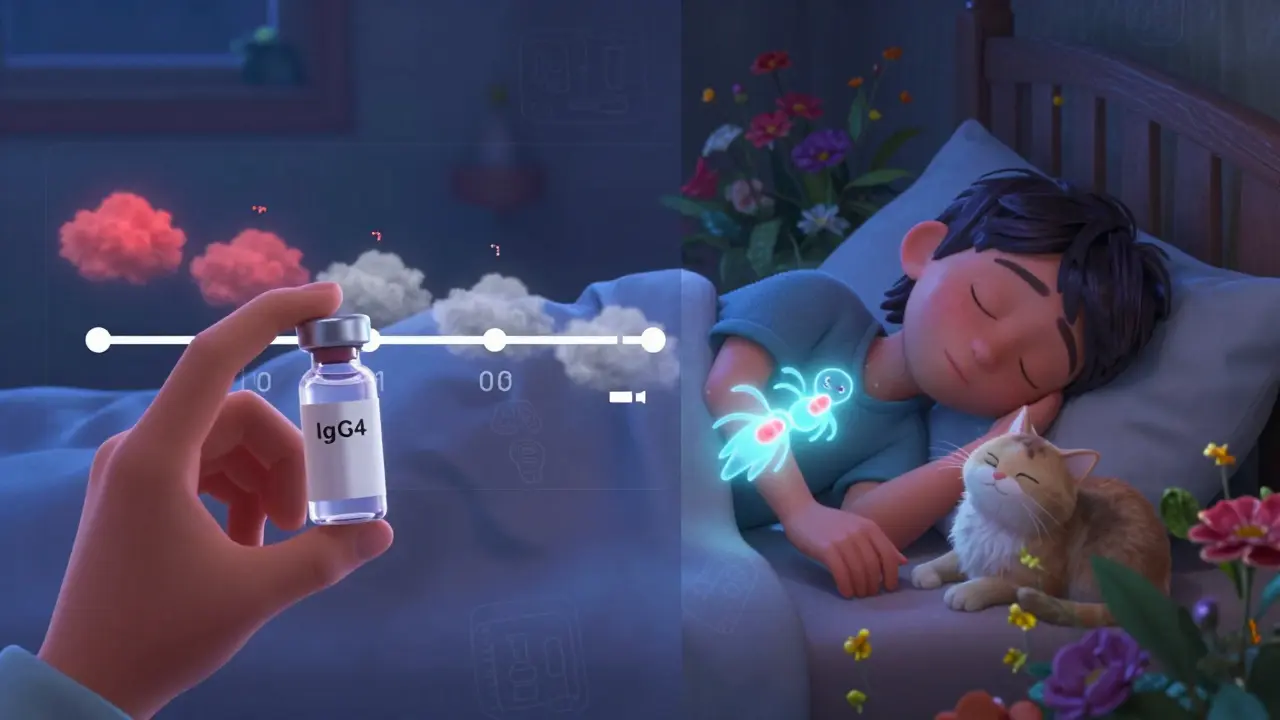
How Immunotherapy Works
Immunotherapy doesn’t just treat allergies - it changes them. The idea is simple: expose your body to tiny, controlled amounts of the allergen you’re sensitive to, then slowly increase the dose. Over time, your immune system learns not to treat it like a threat. Instead of releasing histamine and causing sneezing, itching, or wheezing, it starts to ignore the substance. This shift happens because your body begins producing special antibodies called IgG4, which block the allergic response. It’s like teaching your body to be less afraid.
This approach isn’t new. It was first used in London in 1911 by two doctors treating hay fever. Today, it’s backed by decades of research and is the only allergy treatment proven to alter the disease course. Studies show that after 3-5 years of treatment, many patients see their symptoms cut in half - and some never need medication again. Even better, immunotherapy can reduce the chance of developing new allergies or asthma later on.
Allergy Shots: The Gold Standard
Allergy shots, or subcutaneous immunotherapy (SCIT), are still the most effective option for most people. They involve injections under the skin, usually in the upper arm. You start with very low doses and gradually increase them over weeks or months until you reach a maintenance dose. Once you’re there, you get shots less frequently - often once a month.
The big advantage? Customization. Your allergist can mix multiple allergens into one vial - grass, ragweed, dust mites, cat dander - all in a single shot. That’s critical because 78% of allergy sufferers react to more than one trigger. A 2021 study found allergy shots reduced symptoms by 82% in multi-allergen patients, compared to just 67% for tablets.
There are three ways to build up to the maintenance dose:
- Traditional build-up: Weekly shots for 3-12 months. Low risk of reactions, but time-consuming.
- Cluster build-up: 8-10 visits over 4-9 weeks. Faster, with slightly higher but still safe reaction rates.
- Rush immunotherapy: One long day of multiple shots. Reserved for serious cases like venom allergies.
After reaching maintenance, you continue for 3-5 years. Most people notice improvement within 6-12 months. By year 3, many are off their inhalers, nasal sprays, and antihistamines entirely. The American Academy of Allergy, Asthma & Immunology calls it the only treatment that modifies the immune system itself.

Sublingual Tablets: Convenience Without Compromise?
Sublingual immunotherapy (SLIT) tablets are a newer option. You place a small tablet under your tongue and let it dissolve. No needles. No office visits. Just daily doses at home.
The FDA has approved four tablets so far:
- Oralair: For grass pollen (taken 4 months before and during pollen season)
- Grastek: Also for grass pollen (daily year-round)
- Ragwitek: For ragweed (daily year-round)
- Odactra: For dust mites (daily year-round)
Each tablet targets only one allergen. That’s the catch. If you’re allergic to grass and dust mites, you’d need two tablets. If you’re allergic to three things? No option yet. And while tablets are convenient, they’re less effective for multi-allergen sufferers. A 2023 Reddit analysis of over 1,200 users found that 68% had better results with shots.
Side effects are milder - mostly itchy mouth or throat - but they can be annoying. About 28% of users report oral itching in clinical trials. And if you miss doses? Effectiveness drops sharply. One study showed adherence below 80% cut results in half the benefit.
Still, for people who travel often, have busy schedules, or hate needles, tablets are a game-changer. A 2022 survey found 92% of tablet users preferred them over shots - mostly because they could fit treatment into their daily routine without disrupting work or life.
Which One Is Right for You?
There’s no one-size-fits-all answer. Here’s how to decide:
- Choose allergy shots if: You’re allergic to three or more allergens, your symptoms are severe, you want the best possible results, and you can commit to regular visits.
- Choose sublingual tablets if: You’re allergic to just one thing (like grass or dust mites), you can’t make weekly appointments, and you’re okay with slightly less dramatic improvement.
Experts agree: if you have multiple allergies, shots are the clear winner. Dr. David M. Lang from Cleveland Clinic says, “Subcutaneous immunotherapy remains the most effective long-term treatment for allergic rhinitis.” But if convenience matters more than maximum efficacy, tablets are a valid alternative.
One thing both methods share: they require patience. You won’t see results overnight. It takes months. But for many, the payoff is worth it. One patient wrote in a Google review: “After two years of shots, I went from using three medications daily to none. I finally slept through the night.”
What to Expect During Treatment
If you choose shots, expect to spend time in a clinic. During build-up, you’ll need to stay for 30 minutes after each shot because of the small risk of an allergic reaction. That’s why 32% of patients drop out - they can’t fit it into their schedule. Cluster build-up helps: you can compress months of visits into a few weeks.
For tablets, you’ll need to be disciplined. Set a daily alarm. Don’t skip days. Avoid eating or drinking for five minutes after taking it. And if you feel swelling in your throat or trouble breathing, stop and call your doctor - rare, but possible.
Both treatments require follow-ups. Your allergist will track your progress and adjust your plan if needed. Most clinics now use digital tools to help you log symptoms and adherence.
Cost, Access, and the Future
Allergy shots are covered by most insurance plans, but you’ll still pay copays for each visit. Tablets are pricier upfront - often $200-$400 per month - but you don’t need to go to the doctor as often. Some insurers cover them only after you’ve tried other treatments.
Access is another issue. There are only about 5,300 board-certified allergists in the U.S. Many rural areas have none. That’s why tablets are growing fast - they don’t require a specialist nearby.
The future looks promising. In April 2024, the FDA approved a new tablet for cat dander. More multi-allergen tablets are in Phase 3 trials and could be available by 2026. Researchers are also testing peptide-based treatments that might shorten the course from 3-5 years to just 1-2.
For now, the choice comes down to your needs. If you want the strongest, most comprehensive treatment - and you’re willing to put in the time - shots are still the best option. If you need something simple, safe, and easy to stick with, tablets work well - as long as your allergies are limited to one or two triggers.
Either way, you’re not just treating symptoms. You’re changing your body’s relationship with allergens. And that’s something no pill can do.
How long does immunotherapy take to work?
Most people start noticing improvement within 6 to 12 months, but full benefits usually take 2 to 3 years. The full course lasts 3 to 5 years, regardless of whether you choose shots or tablets. Stopping early can mean losing the benefits.
Are allergy shots safe?
Yes, when done under medical supervision. Traditional build-up has a low risk of serious reactions - about 2.1% of patients. Cluster and rush protocols have slightly higher rates, but clinics are equipped to handle reactions immediately. Anaphylaxis is rare, occurring in fewer than 1 in 1,000 doses.
Can children get immunotherapy?
Yes. Both allergy shots and sublingual tablets are approved for children as young as 5 years old. In fact, starting early can prevent the progression of allergies into asthma. Pediatric allergists often recommend shots for kids with multiple allergies or severe symptoms.
Do I need to stop taking allergy meds during immunotherapy?
No. You can continue using antihistamines, nasal sprays, or inhalers while starting immunotherapy. Many people reduce their medication use over time as their symptoms improve. Your allergist will help you adjust based on your progress.
Is immunotherapy covered by insurance?
Most insurance plans cover allergy shots because they’re considered standard care. Sublingual tablets are covered too, but sometimes only after you’ve tried other treatments. Always check with your provider - copays and prior authorizations vary.
What happens if I miss a shot or tablet dose?
Missing one shot won’t undo progress - your allergist will just adjust your next dose. But missing tablets regularly can cut effectiveness in half. If you miss more than a few days in a row, talk to your doctor before restarting. Consistency matters more than perfection.
Can I switch from tablets to shots later?
Yes. Many people start with tablets for convenience, then switch to shots if their allergies worsen or they develop new sensitivities. There’s no harm in switching - your allergist will design a safe transition plan.
Are there any long-term side effects?
No. Decades of data show immunotherapy is safe over the long term. Unlike long-term steroid use, it doesn’t cause weight gain, bone loss, or immune suppression. The only known long-term benefit is reduced allergy and asthma risk.
Jane Wei
December 18, 2025 AT 06:15Been on SLIT for dust mites for a year-my nose doesn’t feel like a leaky faucet anymore. No needles, no drama.
BETH VON KAUFFMANN
December 19, 2025 AT 08:23Let’s be real-SCIT is the only immunotherapy with Level 1 evidence. SLIT tablets are essentially placebo-grade for polyallergenic patients. The 2021 multi-allergen study showed 82% symptom reduction vs. 67% for SLIT. If you’re allergic to more than two things and think tablets are equivalent, you’re not reading the same papers I am.
Jessica Salgado
December 20, 2025 AT 05:10I started shots after my asthma got worse during pollen season. First six months? Still sneezing. But by month 10, I didn’t need my rescue inhaler. Now, at year 3, I haven’t bought antihistamines in 14 months. It’s not magic-it’s biology. Your immune system forgets how to panic. And honestly? The clinic visits became a weird kind of meditation. I’d sit there, arm out, thinking about how my body was slowly learning not to hate the world.
Radhika M
December 21, 2025 AT 00:58I live in India, and allergy shots are hard to find. My doctor gave me SLIT for grass pollen-it’s expensive, but I take it daily. My eyes don’t water anymore. It’s not perfect, but it’s better than nothing.
Erik J
December 21, 2025 AT 09:17Does anyone know if the new cat dander tablet works for people who also have dust mite sensitivity? I’m allergic to both and I don’t want to take two pills a day. Also, is there data on long-term adherence for SLIT beyond 3 years?
Donna Packard
December 23, 2025 AT 06:36To anyone thinking about starting immunotherapy: just do it. It’s not fun, but it’s worth it. I used to cancel plans because of my allergies. Now I hike. I pet dogs. I open windows. You deserve that.
Victoria Rogers
December 23, 2025 AT 17:06Why are we even talking about this? Shots are just a scam to keep people going to doctors. I tried it. Got a rash. Quit. Now I just use Zyrtec and live my life. Why pay $500 a year for shots when a pill costs $15? We’re being played.
Philippa Skiadopoulou
December 24, 2025 AT 18:31SLIT adherence is critical. A 2023 BMJ meta-analysis showed efficacy drops by 48% when daily dosing falls below 80%. The convenience of tablets is offset by the discipline required. Most users underestimate this.
Raven C
December 25, 2025 AT 11:46It’s amusing how the modern medical establishment has reduced a profound immunological intervention-rooted in over a century of clinical observation-to a consumer choice between ‘needle’ and ‘tablet.’ One is a medical protocol; the other is a lifestyle accessory. I, for one, refuse to treat my immune system like a subscription service.
Steven Lavoie
December 26, 2025 AT 01:46As someone who grew up in rural Alaska with zero allergists nearby, I started SLIT because it was the only option. I’m allergic to birch, ragweed, and mold-so I take two tablets. It’s not ideal, but I’m breathing. The future of multi-allergen tablets can’t come soon enough.
Salome Perez
December 26, 2025 AT 06:42Just want to say thank you for writing this so clearly. My 8-year-old started shots last year-she was terrified of needles, but we did cluster build-up and now she’s proud of her ‘allergy superhero arm.’ She doesn’t even cry anymore. Immunotherapy isn’t just about symptoms-it’s about giving kids their childhood back.
Pawan Chaudhary
December 27, 2025 AT 19:25Here in India, many doctors still don’t know about SLIT. I had to import my tablet from the US. Took 3 months. Worth it. My sneezing stopped. No more running to the pharmacy every spring.
Jody Patrick
December 28, 2025 AT 05:54Shots work. Tablets are for people who hate needles. End of story.
Naomi Lopez
December 29, 2025 AT 09:29Actually, the 2023 Reddit analysis you cited? Total garbage. Over 60% of those users were self-diagnosed, didn’t have skin tests, and didn’t complete treatment. Correlation ≠ causation. Also, ‘Reddit analysis’ isn’t a study. Please stop citing forums like they’re JAMA.