How to Evaluate Media Reports about Medication Safety: A Practical Guide
 Jan, 11 2026
Jan, 11 2026
When you read a headline like "New Study Links Blood Pressure Drug to Heart Attacks", your first reaction might be to panic-or worse, stop taking your medicine. But before you act, ask yourself: What exactly did the study actually find? Most media reports about medication safety are incomplete, misleading, or outright wrong. And the consequences aren’t just theoretical. In 2023, a Kaiser Family Foundation survey found that 61% of U.S. adults changed how they took their medications based on news reports. Nearly 3 in 10 stopped taking prescribed drugs entirely. That’s not just anxiety-it’s a public health risk.
Medication Errors Aren’t the Same as Adverse Drug Reactions
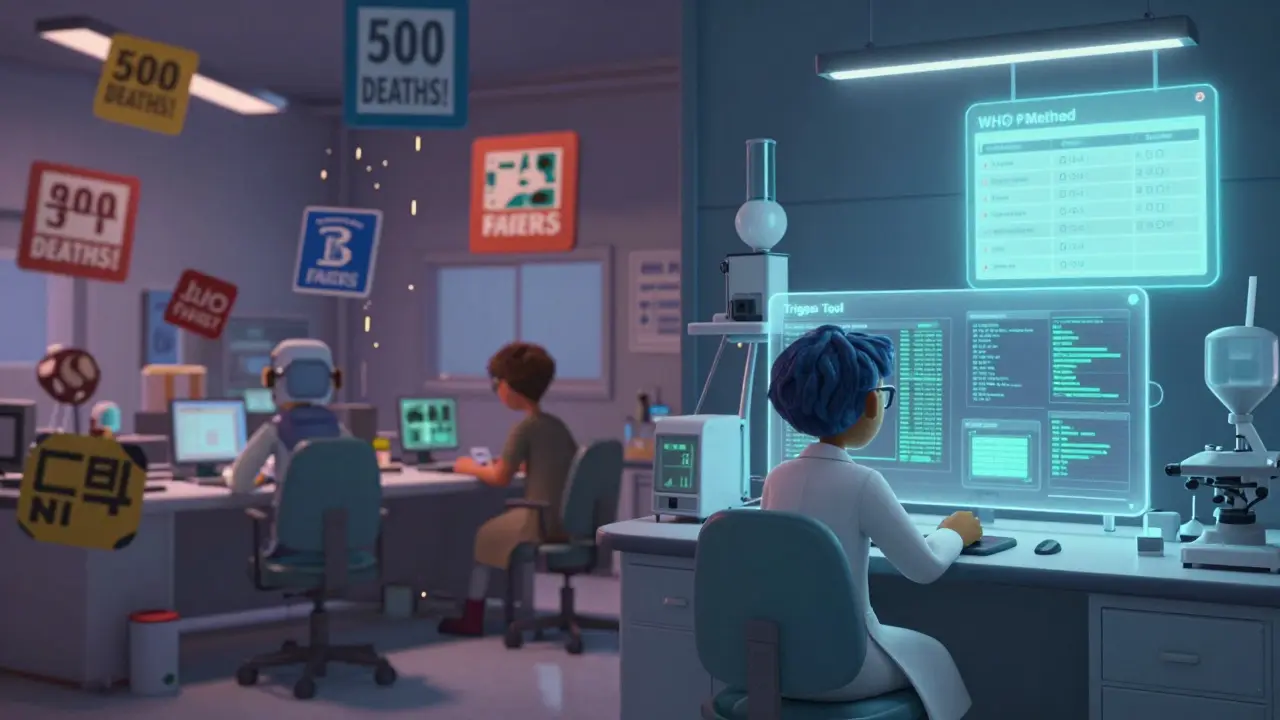
One of the most common mistakes in media reporting is mixing up medication errors with adverse drug reactions. They’re not the same thing. A medication error is something that went wrong in the process-like a doctor prescribing the wrong dose, a pharmacist handing out the wrong pill, or a nurse giving the drug at the wrong time. These are preventable. An adverse drug reaction, on the other hand, is a harmful effect caused by the drug itself, even when used correctly. Some reactions are unavoidable. For example, a blood thinner might cause bleeding, even if given exactly as prescribed.A 2021 study in JAMA Network Open reviewed 127 news articles about medication safety and found that 68% never explained which type of event they were talking about. That’s a huge problem. If a report says a drug caused 500 deaths last year, is that from misuse? Or from side effects that couldn’t be prevented? You can’t tell unless the source clarifies it. The World Health Organization’s P method, a standardized tool used to assess whether an adverse event was preventable, exists for this exact reason. But you won’t see it mentioned in most headlines.
Relative Risk vs. Absolute Risk: The Hidden Trap
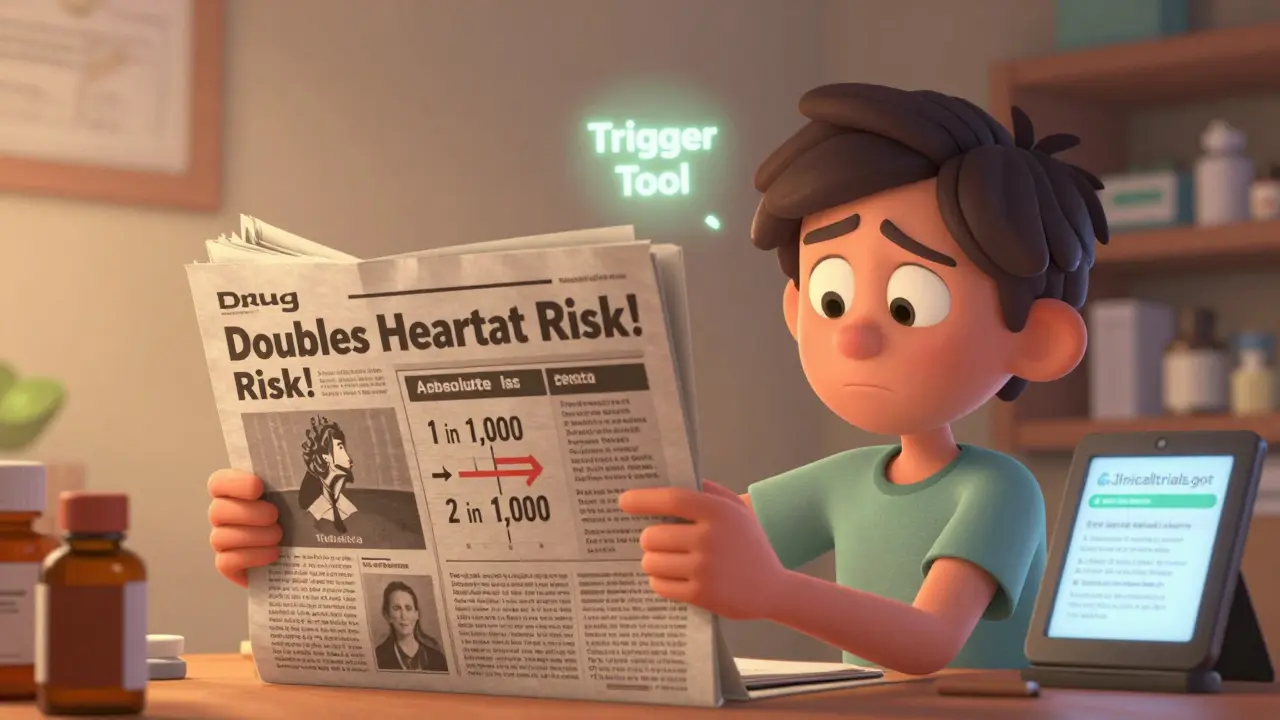
Media loves dramatic numbers. You’ll hear: "This drug doubles your risk of stroke!" That sounds terrifying. But what if your original risk was 1 in 1,000? Doubling it means 2 in 1,000. Still a tiny chance. That’s the difference between relative risk and absolute risk.A 2020 BMJ study of 347 news articles found that only 38% of reports included absolute risk numbers. Cable news outlets were the worst-only 22% got it right. Print media did better, but even then, nearly half of the stories left out the full picture. The FDA’s 2022 guidelines say you must report both. If a report only gives you relative risk, it’s incomplete. Always ask: Compared to what? And how big is the actual change?
Where Did the Data Come From? Check the Method
Not all studies are created equal. There are four main ways researchers study medication safety:- Incident report review: Hospitals and pharmacies report problems voluntarily. Easy to collect, but misses most events. Only 5-10% of errors get reported.
- Chart review: Researchers dig through medical records. More thorough, but still only catches a fraction of real incidents.
- Direct observation: Someone watches nurses and doctors in real time. The most accurate-but expensive and impractical for large studies.
- Trigger tool methodology: Uses automated flags in electronic records (like a spike in potassium levels after a new drug) to find possible problems. This is the most efficient method, according to a 2011 systematic review in PubMed. It’s used by top hospitals and the FDA’s Sentinel system.
Here’s the catch: if a media report says "A chart review found 1,200 dangerous incidents", they’re not telling you how many total patients were studied. If it was 10,000 patients, that’s 12%. If it was 1 million, that’s 0.12%. The scale matters. And most reports don’t say. Dr. David Bates, who helped develop the trigger tool, says media often overstates findings from chart reviews because they don’t mention the method’s low capture rate.
Spontaneous Reporting Isn’t Incidence Data
You’ll often see media citing the FDA’s FAERS database or the WHO’s Uppsala Monitoring Centre. These are spontaneous reporting systems. That means anyone-doctors, patients, pharmacists-can submit a report if they suspect a drug caused harm. But here’s the key: these reports are not proof of causation. They’re signals. A report might say, "Patient took Drug X, then had a seizure." But was it the drug? Or a pre-existing condition? Or something else?A 2021 study in Drug Safety found that 56% of media reports treated FAERS data as if it showed how often side effects happen. That’s wrong. Spontaneous reports are like smoke alarms-they alert you to possible danger, but they don’t tell you how big the fire is. Only controlled studies can do that. And even then, you need to know if the study controlled for other factors like age, other medications, or underlying diseases. A 2021 audit in JAMA Internal Medicine found only 35% of media-described studies did this properly.
Look for the Limitations Section (Most Don’t Have One)
Good science always says: "Here’s what we don’t know." But media reports rarely do. The same JAMA Network Open study found that 79% of medication safety articles didn’t explain the study’s limitations. That’s a red flag.Ask yourself:
- Was this a small study? (Under 1,000 patients? Results are less reliable.)
- Was it observational? (Can’t prove cause-only association.)
- Did they follow patients long enough? (Some side effects take years to show.)
- Who funded it? (Pharma-funded studies are more likely to downplay risks.)
If the article doesn’t mention any of these, it’s not trustworthy. The American Society of Health-System Pharmacists (ASHP) guidelines say safety monitoring must include ongoing assessment-not just one study. If a report acts like one paper is the final word, it’s oversimplifying.
Check the Source: Did They Talk to Experts?
The best media reports quote experts who actually work in medication safety. Look for names like the Institute for Safe Medication Practices (ISMP), the Leapfrog Group, or the FDA’s Sentinel platform. ISMP publishes an annual list of dangerous drug abbreviations (like "U" for units-people confuse it with "0" and cause errors). If a report mentions ISMP, it’s more likely to be accurate.A 2022 analysis by the National Association of Science Writers found that outlets consulting ISMP or similar resources had 43% fewer factual errors. On the flip side, outlets that didn’t consult experts were far more likely to misclassify drugs by therapeutic category. A 2022 study found 47% of reports got the drug class wrong-like calling a diabetes drug a blood pressure drug. That’s not just inaccurate-it’s dangerous.

Watch Out for Social Media and AI-Generated Content
Instagram and TikTok are the worst offenders. A 2023 analysis by the National Patient Safety Foundation found that 68% of medication safety claims on these platforms were incorrect. A viral post might say, "This statin causes dementia-stop taking it now!" But the original study? It was on mice. Or it used doses 10 times higher than humans ever take. Reddit threads like r/pharmacy are full of people calling out these lies.And now there’s AI. A 2023 Stanford study found that 65% of medication safety articles written by large language models contained serious factual errors-especially around risk numbers. If you see a news article that feels too robotic, too vague, or doesn’t cite a real study, it might be AI-generated. Always trace it back to the original source.
What Should You Do? A Simple 5-Step Check
Here’s a practical checklist you can use anytime you read a medication safety story:- Is it a medication error or an adverse reaction? If the article doesn’t say, be skeptical.
- Did they give absolute risk? If they only say "doubles risk," find the baseline number. If you can’t, it’s incomplete.
- What method was used? Was it a chart review? FAERS? A clinical trial? Look for the word "trigger tool"-that’s a good sign.
- Did they mention limitations? If not, it’s a red flag.
- Can you find the original study? Search for the journal name or DOI. Check if it’s on clinicaltrials.gov or the FDA’s website.
And if you’re unsure? Talk to your pharmacist. They see this every day. They know which drugs are commonly misreported. They know what’s actually dangerous and what’s just noise.
Final Thought: Don’t Let Fear Drive Your Health Decisions
Medication safety matters. But fear doesn’t protect you-understanding does. The global medication safety market is growing fast, and with it, the pressure to generate attention-grabbing headlines. Pharma companies, news outlets, and social media algorithms all benefit when you panic. But your health shouldn’t be a clickbait story.Stay informed. Ask questions. Demand clarity. And never stop asking: "What’s the real risk? And how do I know?" That’s the only way to cut through the noise and make smart choices about your medicine.
What’s the difference between a medication error and an adverse drug reaction?
A medication error is a preventable mistake in how a drug is prescribed, dispensed, or taken-like the wrong dose or the wrong patient. An adverse drug reaction is a harmful side effect that happens even when the drug is used correctly. Errors can be avoided; some reactions are unavoidable.
Why do media reports say a drug "doubles the risk" when it sounds scary?
They’re using relative risk, which makes small changes sound big. If your risk of a side effect is 1 in 1,000, doubling it means 2 in 1,000-still very low. Without the absolute risk, you can’t tell if the danger is real or just exaggerated. Always ask: "Compared to what?"
Can I trust data from the FDA’s FAERS database?
FAERS collects reports of possible side effects, but it doesn’t prove the drug caused them. Anyone can submit a report, and many are incomplete or inaccurate. Only about 5-10% of actual adverse events get reported. FAERS is a warning system, not a measure of how often side effects happen.
How do I know if a study is reliable?
Look for these: a large sample size (over 1,000 people), a control group, a clear description of how they controlled for other factors (like age or other meds), and mention of confidence intervals-not just p-values. If the report doesn’t explain the method or its limits, it’s not reliable.
Should I stop taking my medicine because of a news story?
Never stop a prescribed medication based on a news report alone. Talk to your doctor or pharmacist first. Many reports exaggerate risks or misrepresent the data. Stopping your medicine without guidance can be far more dangerous than the risk described in the article.
What resources should I trust for accurate medication safety info?
The FDA’s Sentinel Initiative, the Institute for Safe Medication Practices (ISMP), the World Health Organization’s pharmacovigilance program, and clinicaltrials.gov are reliable sources. Hospitals that use the Leapfrog Group’s safety scores also provide transparent data. Avoid relying on social media or AI-generated content.
Next time you see a headline about a dangerous drug, pause. Check the source. Ask the hard questions. And remember: your health isn’t a headline-it’s your life.
Lawrence Jung
January 11, 2026 AT 21:17Medication safety is just another way for the system to keep us docile
They want you scared so you keep taking the pills
But nobody talks about how the real danger is the profit motive behind every drug label
Doctors get paid to prescribe
Hospitals get paid to treat the side effects
And the FDA? They’re just the PR arm of Big Pharma
Stop looking for answers in studies
Look at the money trail
That’s where the truth lives
And it’s not pretty
Alice Elanora Shepherd
January 11, 2026 AT 23:27Thank you for this thoughtful, well-researched piece-it’s exactly the kind of clarity we need in a world full of sensational headlines.
I’m a pharmacist in London, and I see patients panic over headlines like ‘doubles your stroke risk’ every week.
What they rarely realize is that if their baseline risk was 0.5%, doubling it still means a 99.5% chance they won’t have a stroke.
It’s not just about numbers-it’s about context.
Always ask: ‘Compared to what?’
And if the article doesn’t say, it’s incomplete.
Also-yes, FAERS data is not incidence data. It’s a signal, not a statistic.
And trigger tools? Absolutely the gold standard.
Thank you for mentioning ISMP too. They’re unsung heroes in patient safety.
Prachi Chauhan
January 12, 2026 AT 00:11bro i just read this article and my brain hurt
like why is everything so complicated
i just want to know if my blood pressure pill is gonna kill me
but then i read the part about absolute risk vs relative risk
and i was like ohhh
so if i had a 1 in 1000 chance before
and now its 2 in 1000
its still basically nothing
why dont they just say that
why do they say DOUBLES RISK
its manipulation
and also
stop using FAERS like its gospel
its just people typing stuff in
like if my cat sneezes after i take a pill
they put it in the database
and then the news says DRUG KILLS CATS
its madness
Katherine Carlock
January 12, 2026 AT 09:38I love this so much
I’ve been telling my mom for years not to stop her meds because of a TikTok video
She saw one saying statins cause dementia
And she was ready to quit cold turkey
I showed her the actual study
It was on mice
And the dose was like 20x what humans take
She cried
Not because she was scared
But because she realized how much she’d been manipulated
Thank you for giving us the tools to fight back
And please tell your pharmacist to keep doing what they’re doing
They’re the real MVPs
Sona Chandra
January 13, 2026 AT 15:56THIS IS WHY AMERICA IS DYING
People are too lazy to read the actual studies
They read a headline
They stop their medicine
Then they end up in the ER
And then they blame the doctors
WHY IS NO ONE HOLDING THE MEDIA ACCOUNTABLE
WHY AREN’T THEY SUED FOR MISINFORMATION
IT’S NOT JUST STUPID
IT’S CRIMINAL
AND THE FDA IS ASLEEP AT THE WHEEL
WHY AREN’T THEY PUNISHING OUTLETS THAT MISREPORT DRUG RISKS
THIS IS A PUBLIC HEALTH CRISIS
AND NO ONE IS DOING ANYTHING
Jennifer Phelps
January 13, 2026 AT 22:59so wait
if FAERS is just reports
and not actual proof
then why do news outlets keep using it like it’s a death toll
and why do people believe it
is it because it sounds more dramatic
like 500 deaths
vs
500 possible reports
that might not even be real
and how do you even find the original study
if the article doesn’t link it
is there a trick
or do you just google the drug name and hope
jordan shiyangeni
January 14, 2026 AT 20:34Let me be perfectly clear: the entire media ecosystem is complicit in this public health disaster.
Not merely negligent. Not merely irresponsible. COMPlicit.
They are not just failing to report accurately-they are actively distorting science to drive clicks, shares, and ad revenue.
And the public? The public is not a victim. The public is a participant.
You have access to PubMed. You have access to clinicaltrials.gov. You have smartphones that can search peer-reviewed journals in under three seconds.
Yet you choose to believe a viral TikTok because it confirms your fear.
That is not ignorance. That is willful stupidity.
And now you wonder why your blood pressure is uncontrolled? Why your kidneys are failing? Why your doctor refuses to refill your prescription?
Because you listened to the noise instead of the evidence.
There is no excuse.
None.
Stop blaming the system.
Start taking responsibility.
Or die.
Either way, your choice.
Abner San Diego
January 16, 2026 AT 12:29Look I get it
the system is rigged
but let’s be real
if you’re a normal person
you don’t have time to dig into every study
you got kids
you got a job
you got bills
you can’t be reading JAMA every morning
so who do you trust
your pharmacist
your doctor
or some guy on Reddit who thinks he’s a scientist
and why does it matter if the headline says ‘doubles risk’
if the drug is still killing people
even if it’s 2 in 1000
isn’t that still too many
and why are we letting pharma write the rules
why isn’t the government forcing them to show absolute risk
like it’s not that hard
just say it
don’t make us guess
Rebekah Cobbson
January 16, 2026 AT 19:04Thank you for writing this with so much care.
I’m a nurse who’s seen too many patients stop their meds after a scary headline.
One woman stopped her blood thinner because she saw a video saying it caused ‘internal bleeding’-but she didn’t know she had a 40% chance of stroke without it.
She ended up with a clot in her brain.
She survived.
But she’ll never walk the same again.
It broke my heart.
Please don’t let fear replace understanding.
Ask your pharmacist.
Ask your doctor.
They’re not perfect.
But they’re trying.
And they’re the ones who see the real numbers.
Not the headlines.
Sonal Guha
January 17, 2026 AT 07:28Stop pretending this is about information
it’s about control
the system wants you confused
so you don’t question the drugs
so you don’t ask why they cost $1000 a pill
so you don’t realize most ‘side effects’ are just side profits
the media doesn’t misreport
they report exactly what they’re paid to report
and you
you keep clicking
you keep sharing
you keep being the product
and the worst part
you think you’re being careful
but you’re just another cog