How Smoking and Alcohol Trigger Skin Pain - What You Need to Know
 Oct, 3 2025
Oct, 3 2025
Skin Pain Trigger Calculator
Assess Your Skin Pain Risk
Answer the questions below to calculate your risk level for skin pain triggered by smoking and alcohol.
Your Risk Assessment
Quick Takeaways
- Both smoking and alcohol shrink blood vessels, slowing nutrient delivery to skin.
- Nicotine and acetaldehyde raise inflammation, making skin more sensitive to pain.
- Combined use amplifies oxidative stress, worsening chronic skin discomfort.
- Stopping or reducing use improves wound healing within weeks.
- Seek a dermatologist if pain persists after lifestyle changes.
When you feel a lingering sting or ache on your face, arms, or legs, the culprit is often hidden beneath the surface. Skin Pain is a sensation ranging from mild tingling to sharp burning that signals tissue irritation, inflammation, or nerve involvement. While genetics and environmental factors play a role, two habits stand out for their direct impact: Smoking inhalation of tobacco smoke containing nicotine, tar, and thousands of chemicals and Alcohol consumption of ethanol that metabolizes into acetaldehyde and other toxic by‑products. Understanding how they aggravate smoking skin pain helps you cut the cycle and restore comfort.
How Smoking Fuels Skin Pain
Smoking introduces nicotine straight into the bloodstream. Nicotine Vasoconstriction the narrowing of blood vessels reduces blood flow to the skin by up to 30%, starving cells of oxygen and nutrients. Without adequate circulation, the skin’s repair mechanisms stall, and any existing irritation lingers longer.
Beyond restricted flow, tobacco smoke packs powerful oxidants. These trigger Oxidative Stress an imbalance between free radicals and the body’s ability to neutralize them. The result is damage to collagen fibers, which keep skin elastic. Weakened collagen translates to micro‑tears that send pain signals through cutaneous nerves.
Inflammation skyrockets as well. Smoke chemicals activate Inflammatory Cytokines protein messengers that amplify the immune response like IL‑1β and TNF‑α. Heightened cytokine levels sensitize nerve endings, turning a harmless itch into a burning ache.
Lastly, nicotine interferes with the skin’s barrier lipids. A compromised barrier loses moisture quickly, leading to dryness and cracking-classic triggers for painful flares in conditions such as eczema or psoriasis.
Alcohol’s Role in Skin Discomfort
Alcohol follows a different biochemical path but arrives at a similar destination: irritated skin. Once consumed, ethanol converts to Acetaldehyde a highly reactive metabolite that damages proteins and DNA. Acetaldehyde accumulates in skin cells, prompting an inflammatory cascade akin to that caused by tobacco.
Alcohol also promotes dehydration. Even moderate drinking can reduce skin water content by 10-15%, stripping away the natural lubricants that keep nerves calm. Dehydrated skin is more prone to fissures, which expose nerve endings and cause sharp pains.
Another overlooked effect is the impact on the liver’s ability to detoxify. A stressed liver struggles to clear inflammatory mediators, allowing them to circulate longer and intensify skin sensitivity.
Heavy drinkers often develop rosacea‑like flushing. The dilation of facial blood vessels during a night out may feel like a throbbing heat, and repeated episodes can evolve into persistent burning sensations.
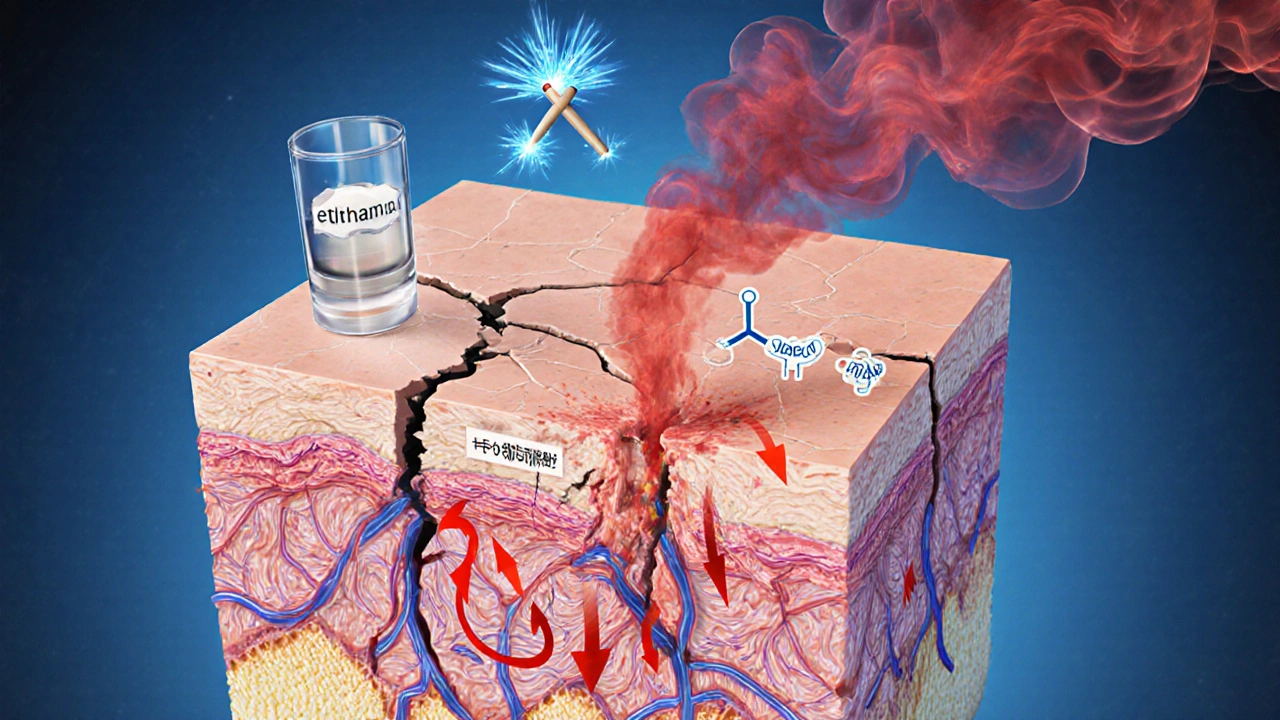
Combined Impact - When Two Vices Meet
Smoking and alcohol share several pathways: both reduce blood flow, increase oxidative stress, and raise inflammatory markers. When used together, these effects are not merely additive; they synergize.
For example, nicotine‑induced vasoconstriction limits the skin’s ability to clear acetaldehyde, prolonging its toxic stay. Simultaneously, alcohol‑driven dehydration weakens the skin’s barrier, making it easier for smoke particles to penetrate deeper.
Research from the British Dermatology Society (2024) showed that dual users reported skin pain intensity scores 40% higher than those who only smoked or only drank. Healing times for minor cuts extended from an average of 5 days to 9 days, highlighting the compounded delay in tissue repair.
| Factor | Smoking | Alcohol |
|---|---|---|
| Blood Flow | Vasoconstriction - reduces flow 30% | Transient dilation followed by dehydration |
| Inflammation | ↑ Cytokines (IL‑1β, TNF‑α) | ↑ Acetaldehyde‑induced cytokines |
| Oxidative Stress | Free radicals from tar | Acetaldehyde creates ROS |
| Collagen Damage | Direct collagen breakdown | Impaired synthesis via liver stress |
| Pain Frequency | Intermittent burning, especially after exposure | Throbbing after binge episodes |
Practical Steps to Ease the Burn
- Cut back gradually. Even reducing daily cigarettes by one pack can improve microcirculation within two weeks.
- Limit alcohol to ≤1standard drink per day for women and ≤2 for men. Alternate with water to keep skin hydrated.
- Boost your skin’s barrier: use ceramide‑rich moisturizers twice daily. Look for products that mention “repair barrier” on the label.
- Eat antioxidant‑rich foods - berries, leafy greens, and nuts - to counteract free radicals from smoke and alcohol.
- Stay active. Light cardio (walking, cycling) promotes blood flow and helps flush toxins.
- Consider nicotine‑replacement therapy if quitting feels overwhelming. Patches or gum reduce withdrawal‑related stress that can worsen skin pain.
Consistency is key. Most users notice a measurable drop in pain intensity after four to six weeks of combined lifestyle changes.
When to Call a Professional
If you experience any of the following, schedule a dermatologist appointment promptly:
- Persistent burning that lasts more than two weeks despite DIY care.
- Open sores or ulcers that don’t close within ten days.
- Sudden changes in skin color, such as unexplained redness or bluish patches.
- Accompanying symptoms like fever, swelling, or joint pain.
Doctors may perform a skin biopsy, blood tests for inflammatory markers, or recommend prescription‑strength topical steroids to break the pain cycle.
Frequently Asked Questions
Can occasional smoking still cause noticeable skin pain?
Yes. Even light smoking narrows blood vessels temporarily, which can trigger a brief tingling or burning sensation, especially on already sensitive areas like the cheeks or hands.
Is it safe to use over‑the‑counter pain creams while quitting smoking?
Generally, yes. Topical NSAID gels or capsaicin creams act locally and don’t interfere with nicotine metabolism. However, check the label for any skin‑sensitizing ingredients that could worsen irritation.
How long does it take for skin to heal after I quit smoking?
Blood flow improves within 48hours, but noticeable reduction in chronic skin pain usually appears after 2-4weeks. Full recovery of collagen structure can take several months, depending on age and overall health.
Does red wine affect skin pain more than spirits?
Red wine contains polyphenols that can be anti‑inflammatory, but the alcohol content still leads to dehydration and acetaldehyde buildup. Spirits usually have higher alcohol‑by‑volume, so they can cause a sharper flare‑up.
Are there any natural remedies that counteract nicotine‑induced skin pain?
Aloe vera gel, green tea extracts, and omega‑3 supplements have shown modest benefits in soothing inflamed skin and improving barrier function, making nerve endings less reactive.
Edward Webb
October 3, 2025 AT 23:21It is striking how habits that we often deem harmless can, in fact, be insidious architects of chronic discomfort. When you consider the cascade that begins with nicotine’s vasoconstrictive grip, you quickly realise that skin is deprived of the oxygen and nutrients essential for repair. This deprivation does not simply cause a fleeting tingling; it sets the stage for persistent inflammation that sensitises peripheral nerves. Likewise, ethanol, through its metabolite acetaldehyde, introduces a parallel pathway of oxidative stress that compounds the problem. The literature, especially the recent British Dermatology Society report of 2024, underscores a synergistic amplification when both substances are used together. In such dual‑exposure scenarios, the skin’s barrier lipids are eroded, making the epidermis porous to further irritants. The compromised barrier then loses moisture at an accelerated rate, turning the skin from a resilient shield into a desiccated canvas prone to cracking. Cracks, as you know, expose nociceptors directly to the environment, which translates into sharp, localized pain. Moreover, the inflammatory cytokines-IL‑1β, TNF‑α-released in response to both smoke and alcohol act as messengers that perpetuate the pain loop, even after the initial insult has waned. From a philosophical standpoint, this highlights a profound truth: our bodies embody the sum of our choices, and short‑term gratifications can seed long‑term suffering. Yet the narrative is not wholly bleak; the body possesses a remarkable capacity for regeneration once the offending agents are reduced or removed. Microcirculation begins to improve within 48 hours of smoking cessation, and skin hydration can be restored with diligent moisturizing. Antioxidant‑rich foods provide the necessary substrates for the skin to counteract free radicals that accrued during the period of exposure. Light aerobic activity further stimulates blood flow, delivering these reparative nutrients to the dermal layers. Therefore, a structured plan-gradual reduction of cigarettes, moderation of alcohol intake, balanced nutrition, and regular movement-constitutes a pragmatic roadmap to alleviate skin pain. Finally, should the discomfort persist beyond a few weeks despite these interventions, seeking a dermatologist’s expertise remains a prudent step. In essence, understanding the mechanistic interplay between smoking, alcohol, and skin pain empowers you to reclaim comfort and health.
Snehal Suhane
October 12, 2025 AT 08:20Oh great, because wh0 doesn't love a side of burning skin with their cocktail, right?
Ernie Rogers
October 20, 2025 AT 17:18Our great nation thrives when we take care of our bodies and ditching those nasty habits is a small but mighty step toward stronger skin.
Eunice Suess
October 29, 2025 AT 01:17Imagine the agony of a cracked cheek, the tears of a wounded dermis crying out for relief- it is a tragic tableau that demands immediate, dramatic intervention!
Anoop Choradia
November 6, 2025 AT 10:16While the mainstream discourse lauds moderation, it is essential to recognise that the pharmaceutical industry covertly downplays the synergistic damage of tobacco and alcohol to sustain their lucrative market in synthetic analgesics.
bhavani pitta
November 14, 2025 AT 19:15Contrary to such insinuations, the evidence presented by peer‑reviewed dermatological studies adheres to rigorous methodology, rendering any insinuation of intentional suppression unfounded.
Brenda Taylor
November 23, 2025 AT 04:14Honestly, if you keep poisoning yourself, don't be surprised when your skin screams – 🙄
Taryn Thompson
December 1, 2025 AT 13:12The recommendations outlined in the article are sound: reduce nicotine intake gradually, limit alcoholic beverages to no more than one standard drink per day for women and two for men, and reinforce the skin barrier with ceramide‑rich moisturizers. Additionally, incorporating antioxidant‑dense foods such as blueberries, kale, and walnuts can mitigate oxidative stress. Regular, low‑impact cardio improves peripheral circulation, further supporting tissue repair. Should pain persist beyond four weeks despite adherence to these measures, a dermatologist can evaluate for underlying neuropathic conditions and prescribe appropriate topical or systemic therapies.
Gary Tynes
December 9, 2025 AT 22:11Hey man you got this you can cut back step by step and feel the pain fade you just gotta stick with it trust me
Stanley Platt
December 18, 2025 AT 07:10Indeed, your determination is commendable; however, remember to hydrate adequately (≥2 L of water daily) and to schedule regular check‑ins with a healthcare professional-this will optimise your recovery trajectory! 😊
Alice Settineri
December 26, 2025 AT 16:09Whoa, the skin's like a drama queen when you feed it cigarettes and booze-one minute it's glowing, the next it's throwing a full‑blown tantrum, and trust me, nobody enjoys that kind of spectacle!
nathaniel stewart
January 12, 2026 AT 22:21Keep pushing forward, and soon you'll see your skin bounce back brighter than ever-just give it a lil' time!