Compare Deltasone (Prednisone) with Alternatives: What Works Best for Inflammation and Autoimmune Conditions
 Nov, 18 2025
Nov, 18 2025
Prednisone Tapering Calculator
Calculate Your Safe Prednisone Tapering Schedule
Prednisone must be tapered gradually to prevent adrenal crisis. This tool helps you create a safe tapering plan based on your current dose and how long you've been taking prednisone. Always consult your doctor before making any changes to your medication.
When your body’s immune system goes into overdrive-whether it’s from rheumatoid arthritis, asthma, or a severe allergic reaction-doctors often reach for Prednisone. It’s the brand name Deltasone that many patients recognize, but it’s the same active ingredient: prednisone, a powerful synthetic corticosteroid. It works fast. It reduces swelling, calms immune attacks, and can turn a life-threatening flare into something manageable. But it’s not without cost. Long-term use brings weight gain, bone loss, mood swings, and higher risk of infections. That’s why so many people ask: Are there safer or more sustainable alternatives?
How Prednisone Works and Why It’s Still Used
Prednisone mimics cortisol, the natural hormone your adrenal glands make to handle stress. By flooding your system with this synthetic version, it shuts down inflammatory pathways. For conditions like lupus, Crohn’s disease, or severe eczema, it’s often the most effective tool available. In emergency situations-like anaphylaxis or acute spinal cord inflammation-it’s life-saving.
But here’s the catch: prednisone doesn’t discriminate. It doesn’t just quiet the bad inflammation; it dampens your entire immune response. That’s why patients on long-term therapy get sick more often, develop cataracts, or experience muscle wasting. The NHS guidelines recommend the lowest possible dose for the shortest time. Yet, many patients stay on it for months or years because other treatments either don’t work or take too long to kick in.
Alternative 1: Methylprednisolone (Medrol)
Methylprednisolone is chemically very similar to prednisone, but it’s slightly more potent and acts faster. It’s often used in hospital settings for acute flares-think IV drips in emergency rooms or high-dose pulses for multiple sclerosis relapses. Oral Medrol tablets are available, and some doctors prefer them over prednisone for short bursts because they’re absorbed more efficiently.
But here’s the thing: it’s still a corticosteroid. All the same side effects apply. The difference isn’t safety-it’s timing and delivery. If you need a quick, strong hit, methylprednisolone might be the better choice. If you’re on a maintenance plan, prednisone is usually cheaper and just as effective.
Alternative 2: Hydrocortisone
Hydrocortisone is the closest thing to your body’s own cortisol. It’s much weaker than prednisone-about 1/5th the potency. That’s why you see it in over-the-counter creams for rashes. But oral hydrocortisone is used for adrenal insufficiency (Addison’s disease) and sometimes for mild autoimmune conditions in patients who can’t tolerate stronger steroids.
It’s not a replacement for prednisone in moderate to severe cases. If you’re trying to control a flare of ulcerative colitis or polymyalgia rheumatica, hydrocortisone won’t cut it. But for someone who needs only a tiny anti-inflammatory nudge-maybe someone with mild allergic asthma or a skin condition-hydrocortisone can be a gentler starting point.
Alternative 3: Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
Drugs like ibuprofen, naproxen, and celecoxib are the first line for everyday pain and inflammation. They block enzymes (COX-1 and COX-2) that produce prostaglandins-the chemicals that cause swelling and pain. They’re great for arthritis, sprains, or headaches.
But they don’t touch autoimmune inflammation the way steroids do. If your immune system is attacking your joints, lungs, or kidneys, NSAIDs won’t stop the damage. They only mask symptoms. Many patients take NSAIDs alongside low-dose prednisone to reduce the steroid amount needed. But relying on them alone for conditions like vasculitis or systemic lupus is risky and ineffective.

Alternative 4: Disease-Modifying Antirheumatic Drugs (DMARDs)
This is where the real shift happens-from symptom control to disease control. DMARDs like methotrexate, sulfasalazine, and leflunomide work slowly-weeks to months-but they actually change the course of autoimmune diseases. They don’t just calm inflammation; they slow or stop the immune system’s attack on your body.
For rheumatoid arthritis, psoriatic arthritis, or even some forms of lupus, DMARDs are the gold standard for long-term management. Many patients start on prednisone to get immediate relief while waiting for their DMARD to kick in. Once the DMARD takes effect, doctors aim to taper off prednisone completely. Studies show that combining methotrexate with low-dose steroids leads to better outcomes and fewer side effects than steroids alone.
Alternative 5: Biologics and Targeted Therapies
These are the newest and most precise tools. Biologics like adalimumab (Humira), rituximab (Rituxan), and tocilizumab (Actemra) target specific parts of the immune system-like TNF-alpha or B-cells-instead of blasting everything. They’re used when DMARDs fail or when the disease is aggressive.
They’re expensive. They require injections or infusions. And they come with their own risks: higher chance of serious infections, rare neurological side effects, and possible reactivation of old TB or hepatitis. But for patients who’ve tried everything else, they offer a path to remission without the weight gain, mood crashes, or bone thinning that comes with long-term steroids.
A 2024 study in the British Journal of Rheumatology followed 1,200 patients with moderate to severe rheumatoid arthritis. Those switched from long-term prednisone to biologics saw a 68% reduction in fracture risk over three years and a 40% drop in hospitalizations due to infections.
When to Consider Alternatives
There’s no one-size-fits-all answer. But here’s when you should talk to your doctor about stepping away from prednisone:
- You’ve been on it longer than 3 months
- You’re taking more than 5mg per day
- You’ve gained more than 5kg since starting
- You’re developing high blood pressure, diabetes, or cataracts
- You’ve had two or more infections in the past year
These aren’t just side effects-they’re warning signs. The goal isn’t to avoid steroids entirely (they’re essential in emergencies), but to use them as a bridge, not a permanent solution.
What About Natural Alternatives?
Curcumin from turmeric, omega-3s from fish oil, and vitamin D get a lot of attention online. Some small studies suggest they have mild anti-inflammatory effects. But don’t confuse mild with meaningful.
One 2023 trial tested 1,200mg of curcumin daily in patients with osteoarthritis. It reduced pain slightly-about the same as a low-dose NSAID-but had zero effect on joint damage or autoimmune markers. Fish oil helped reduce morning stiffness in rheumatoid arthritis, but not enough to replace methotrexate.
Natural doesn’t mean safe. Turmeric can interfere with blood thinners. High-dose fish oil raises bleeding risk. Vitamin D deficiency is common in autoimmune patients, but supplementing won’t fix the disease. These can support your health, but they’re not replacements for proven medical treatments.
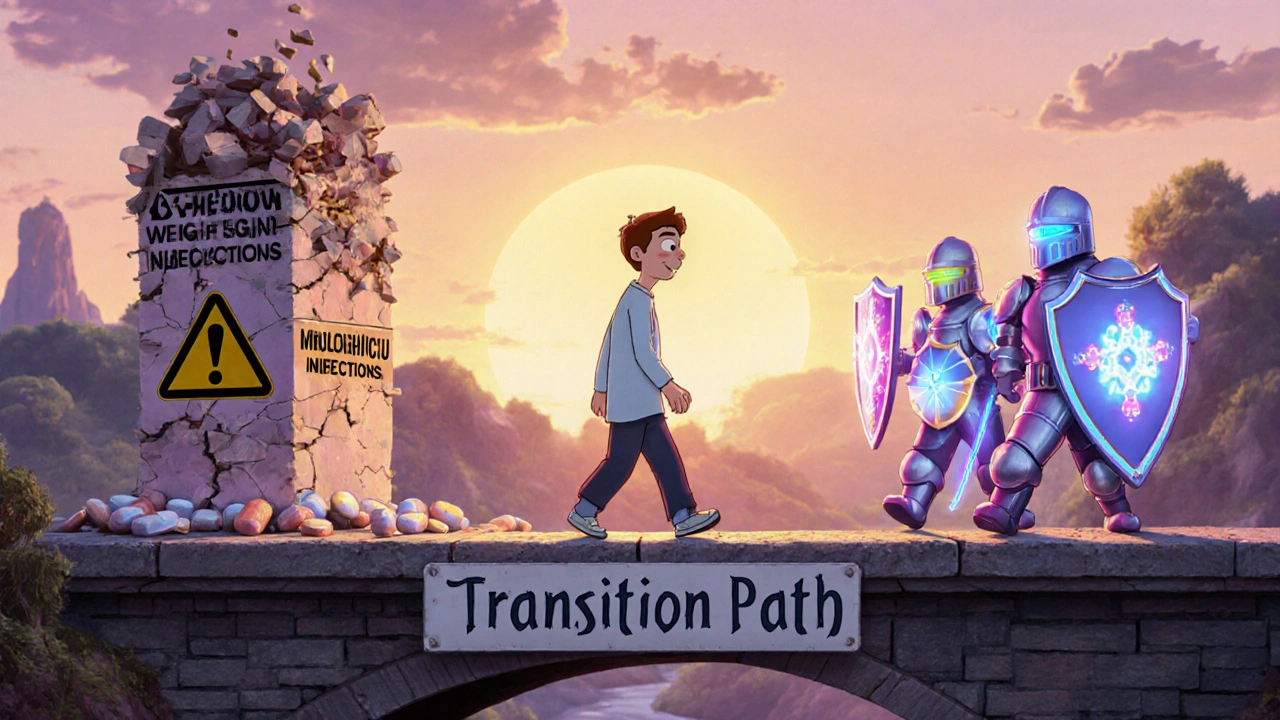
How to Safely Transition Off Prednisone
Never stop prednisone cold turkey. Your adrenal glands shut down after months of external steroid use. Suddenly removing it can cause adrenal crisis-low blood pressure, vomiting, confusion, even death.
The taper must be slow. For someone on 10mg/day for six months, a typical plan might be:
- Reduce by 1mg every 1-2 weeks until reaching 5mg/day
- Then reduce by 0.5mg every 2-4 weeks
- Below 5mg, slow down even more-0.25mg every 3-6 weeks
Your doctor will monitor your symptoms and may check cortisol levels during the process. If you feel dizzy, fatigued, or nauseous during a taper, it’s a sign you’re going too fast. Hold the dose, don’t rush.
Final Thoughts: Choosing the Right Path
Prednisone is a powerful tool, not a villain. But it’s not meant to be a lifelong crutch. The best outcomes come when it’s used as a temporary shield while stronger, targeted therapies take over.
If you’re on Deltasone or generic prednisone and you’re worried about side effects, ask your doctor:
- Can I start a DMARD or biologic to reduce my steroid dose?
- Is there a way to monitor my bone density or blood sugar while I’m on this?
- What’s the plan to get me off prednisone safely?
The goal isn’t just to feel better today-it’s to stay healthy tomorrow. There are better, longer-term options. You just need to start the conversation.
Reema Al-Zaheri
November 18, 2025 AT 18:14Prednisone is a double-edged sword: effective, yes-but the long-term trade-offs are staggering. I’ve seen patients develop avascular necrosis after just 18 months on 10mg/day. The medical community needs to prioritize DMARDs earlier, not later. Waiting until the bones are crumbling is not a strategy-it’s negligence.
Codie Wagers
November 20, 2025 AT 00:24Let’s be honest-this whole system is a pyramid scheme disguised as medicine. Pharma makes billions off steroid dependence, while doctors, pressured by time and insurance, keep prescribing the quick fix. We don’t need alternatives-we need a complete overhaul of how chronic illness is managed. The system is broken, and prednisone is just the symptom.
Paige Lund
November 21, 2025 AT 00:48So… we’re supposed to be impressed that biologics cost $20,000 a year and still make you sick? Cool. Thanks for the info, Doctor.
Zac Gray
November 21, 2025 AT 14:57I get it-you’re scared of steroids. I was too. But here’s the truth: if you’re in pain so bad you can’t hold your coffee cup, prednisone is the only thing that lets you live until the real treatment kicks in. The goal isn’t to fear it-it’s to use it like a scalpel, not a sledgehammer. Taper smart. Monitor close. Pair it with methotrexate. And don’t let anyone make you feel guilty for needing it when you need it.
Steve and Charlie Maidment
November 22, 2025 AT 17:44Why do we even talk about natural alternatives? Because people are desperate. And when you’re told your only options are a chemical wrecking ball or a $30,000 injection, you start Googling turmeric. I’m not saying it works-but I’m saying the system failed them before they ever typed ‘curcumin for lupus’ into Google.
Michael Petesch
November 23, 2025 AT 02:47In Japan, corticosteroid use is far more conservative, with DMARD initiation often occurring within weeks of diagnosis. The cultural emphasis on preventive care and patient education results in significantly lower long-term steroid dependency. This suggests that the issue is not merely pharmacological-but systemic, educational, and cultural. Perhaps we need to look beyond the pill bottle.
Ellen Calnan
November 24, 2025 AT 03:42I was on prednisone for 22 months. Lost 18 pounds of muscle. Had a panic attack every time I saw a pharmacy. Then my rheumatologist switched me to adalimumab-and for the first time in five years, I slept through the night. Not because I’m brave. Not because I’m lucky. Because someone finally listened. If you’re reading this and you’re still on steroids-please, please, please ask for a plan. You don’t have to live like this. There’s another way. I’m proof.
Richard Risemberg
November 25, 2025 AT 08:54Let’s stop calling them ‘alternatives’-they’re not side notes. They’re the main event. Prednisone is the emergency flare gun; DMARDs and biologics are the entire fire department. We’ve been lighting matches and yelling ‘someone call 911!’ while ignoring the hose in the corner. It’s time to stop romanticizing the quick burn and start investing in the real solution. The body doesn’t need a sledgehammer-it needs a surgeon. And we’ve got the tools. Now we just need the will.