Azoles and Tacrolimus: How Drug Interactions Cause Dangerous Level Spikes and Kidney Damage
 Nov, 1 2025
Nov, 1 2025
Tacrolimus-Azole Interaction Calculator
Calculate Safe Tacrolimus Dose Adjustment
When starting an azole antifungal with tacrolimus, proper dose reduction is critical to prevent kidney damage. Enter your current tacrolimus dose and select the azole to calculate the appropriate adjustment.
When a transplant patient gets an infection, doctors often reach for an azole antifungal like voriconazole or posaconazole. It’s effective, widely available, and often given orally. But if that same patient is on tacrolimus - which most solid organ transplant recipients are - a silent danger is lurking. The azole doesn’t just fight the fungus. It also causes tacrolimus levels in the blood to skyrocket, sometimes within days. And when tacrolimus climbs too high, it doesn’t just sit there. It starts damaging the kidneys. This isn’t a rare edge case. It’s a daily reality in transplant clinics across the U.S. and Europe.
Why Azoles and Tacrolimus Don’t Mix
Tacrolimus is a powerful immunosuppressant. It keeps the body from rejecting a new kidney, liver, or lung. But it’s also a narrow therapeutic drug. That means the difference between the right dose and a dangerous one is small. The body breaks down tacrolimus mostly through the liver, using an enzyme called CYP3A4. If that enzyme is blocked, tacrolimus piles up in the bloodstream. Azole antifungals - ketoconazole, itraconazole, voriconazole, posaconazole - are strong inhibitors of CYP3A4. They bind to the enzyme like a key jammed in a lock. The enzyme can’t do its job. Tacrolimus doesn’t get cleared. Levels climb. Studies show that when voriconazole is added, tacrolimus levels can jump 100% to 300%. With ketoconazole, the rise can be even worse - up to 500%. That’s not a slight adjustment. That’s a medical emergency waiting to happen.What Happens When Tacrolimus Levels Spike
High tacrolimus doesn’t just make lab numbers look bad. It directly harms the kidneys. The drug causes blood vessels in the kidneys to constrict. Blood flow drops. The filtering units - glomeruli - get stressed. Creatinine rises. GFR falls. In just 48 hours, a patient’s kidney function can crash. One kidney transplant recipient on a patient forum described it this way: “My levels went from 6.5 to 18.2 overnight. My creatinine doubled. I ended up in the hospital.” This isn’t just about acute injury. Chronic high levels lead to permanent scarring of kidney tissue. The damage can be irreversible. Even after the azole is stopped and tacrolimus is lowered, the kidneys may never fully recover. In transplant centers, azole-tacrolimus interactions are responsible for 15% to 20% of all tacrolimus-related kidney damage cases. That’s not a footnote. That’s a leading cause of post-transplant kidney dysfunction.Not All Azoles Are the Same
Some azoles are worse than others. Ketoconazole is the most dangerous - it’s so potent at blocking CYP3A4 that most transplant centers ban it entirely in tacrolimus patients. Voriconazole is next in line. It’s commonly used for aspergillosis, but its interaction risk is high enough that many pharmacists now treat it like a red flag. Then there’s isavuconazole. It’s newer. And it’s much gentler on CYP3A4. Studies show it only increases tacrolimus levels by 30% to 50%. That’s manageable. But here’s the catch: insurance often won’t cover isavuconazole as a first-line drug. It’s more expensive. So even though it’s safer, patients still get voriconazole because it’s cheaper - and riskier. Echinocandins like micafungin and caspofungin don’t touch CYP3A4 at all. They’re often the best alternative. But they’re IV-only. That’s fine in the hospital. Not so great for outpatient prophylaxis. Amphotericin B is another option, but it has its own kidney toxicity. So you’re trading one risk for another.
How Clinics Are Trying to Fix This
The solution isn’t to avoid antifungals. It’s to manage the interaction. And the best way to do that is with a plan. Most top transplant centers now use standardized protocols. When an azole is started, tacrolimus is cut by 50% to 75%. For isavuconazole, maybe only 25%. Then, daily blood tests for the first week. Trough levels checked every day until stable. Once levels settle, testing drops to two or three times a week. This isn’t optional. It’s mandatory. One transplant pharmacy team in Chicago reported that after implementing a protocol of reducing tacrolimus by 75% when starting posaconazole, they cut toxicity events by 60% in two years. That’s not luck. That’s protocol. Electronic health records now often have alerts built in. If a doctor orders voriconazole for a patient on tacrolimus, the system pops up: “High-risk interaction. Reduce tacrolimus dose by 70%. Monitor levels daily.” But not all hospitals have these alerts. And even when they do, busy clinicians sometimes override them. That’s where the real risk lies.The Human Cost
Behind every lab value is a person. A 58-year-old who got a liver transplant five years ago. She’s been stable. No rejection. No infections. Then she develops a fungal sinus infection. She’s put on voriconazole. Three days later, she’s dizzy, nauseated, her urine output drops. Her creatinine spikes. She’s admitted for acute kidney injury. She needs dialysis for a week. Her tacrolimus dose is cut. She’s terrified. Will her liver reject? Will her kidneys recover? This isn’t rare. A 2022 survey of 127 transplant pharmacists found that 76% saw at least one unplanned hospital admission per month because of this interaction. These aren’t theoretical risks. They’re daily emergencies. And the emotional toll? Patients report anxiety every time they get a new prescription. “I don’t take anything new without checking with my transplant team,” one patient wrote. “I’ve seen what happens when you don’t.”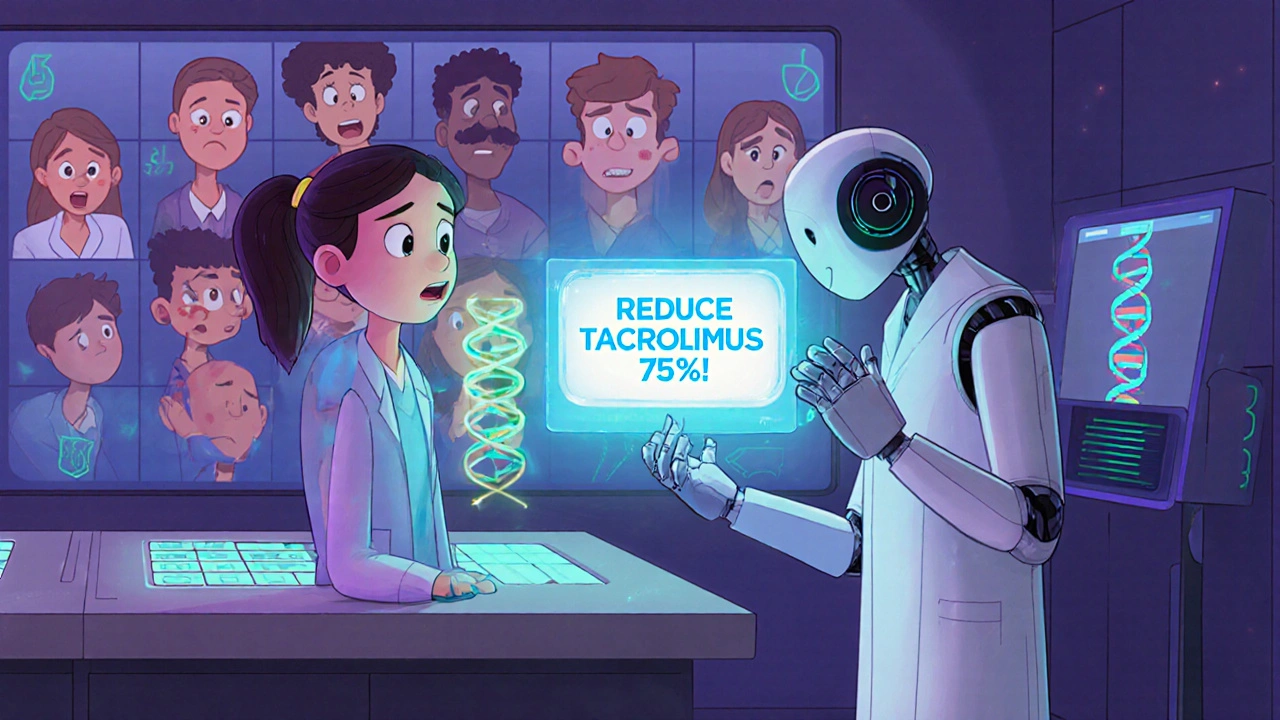
What’s Changing Now
There’s new hope. In 2023, the FDA approved a new extended-release version of tacrolimus. It releases the drug more slowly. That means fewer spikes in blood levels - even if an azole is added. Early data suggests it may reduce nephrotoxicity by 20% compared to the old immediate-release form. There’s also growing interest in genetics. About half of people of African descent carry a gene variant (CYP3A5*3) that makes them “expressers.” Their bodies break down tacrolimus faster. So they need higher doses. But when you add an azole, their levels still rise - just not as dramatically as in non-expressers. In 2024, new guidelines will start recommending genetic testing before starting azoles in high-risk patients. It’s not standard yet. But it’s coming. And then there’s the shift away from calcineurin inhibitors altogether. Drugs like belatacept don’t rely on CYP3A4. No interaction with azoles. But belatacept isn’t for everyone. It’s more expensive. It requires weekly infusions. And it’s not as effective in all transplant types. So tacrolimus remains the backbone of immunosuppression.What You Need to Do
If you’re a transplant patient on tacrolimus:- Never start a new antifungal without talking to your transplant team.
- Ask: “Is this azole necessary? Is there a safer alternative?”
- If you must take an azole, expect your tacrolimus dose to be cut - often by half or more.
- Know your numbers. Ask for your tacrolimus trough level before and after starting the antifungal.
- Watch for signs of kidney trouble: less urine, swelling in legs, fatigue, nausea, confusion.
- Don’t assume your pharmacist or doctor knows the interaction. Bring it up yourself.
- Always check for tacrolimus before prescribing any azole.
- Use a protocol. Don’t wing it.
- Reduce tacrolimus by 50-75% for voriconazole or posaconazole. By 75-80% for ketoconazole (if unavoidable).
- Check levels daily for the first 3-5 days.
- Consider isavuconazole if cost allows.
- Advocate for CYP3A5 genotyping in high-risk patients.
Final Reality Check
This interaction isn’t going away. Transplant numbers are rising. Infections are still a top cause of death in the first year. Azoles are still the go-to for fungal threats. So the risk remains. But the good news? It’s preventable. With knowledge, protocols, and vigilance, these spikes don’t have to lead to kidney failure. The tools are there. The science is clear. The question is whether we’re willing to use them.Because in transplant care, the difference between a safe outcome and a life-altering complication often comes down to one question: Did someone check the interaction?
Sonia Festa
November 3, 2025 AT 02:32Ugh, another one of those ‘just check your meds’ posts. Like anyone actually has time to Google every single drug combo before swallowing a pill. My aunt got dialysis because her doctor didn’t even *ask* if she was on antifungals. Just assumed. Now she’s on a waiting list. Thanks, healthcare system.
Sara Allen
November 3, 2025 AT 05:48Y’all are overreacting. In America we have the BEST doctors and the BEST meds. If your kidney fails it’s cuz you’re lazy or didn’t eat right. Azoles? Pfft. My cousin took voriconazole for 6 months and his kidneys were fine. Probably just drank too much soda.
Amina Kmiha
November 5, 2025 AT 01:49THEY KNOW. THEY KNOW AND THEY DON’T CARE. 🤫💉
Big Pharma *wants* you to need dialysis. It’s a cash cow. Look at the stock prices of kidney dialysis companies - they’re SPiking right after new azole guidelines drop. And the FDA? Paid off. They approved isavuconazole… but only after 12 years of patients dying. Coincidence? 😏
They’re letting you get sick so they can sell you more meds. Wake up.
Ryan Tanner
November 5, 2025 AT 19:47Yo this is actually super helpful. I’ve got a buddy who just got a liver transplant and he’s terrified of every new prescription. Sharing this with him right now. You’re basically the unsung hero of transplant care. 🙌
Also - if you’re on tacrolimus, keep a note on your phone: ‘DON’T TAKE AZOLES WITHOUT TALKING TO YOUR PHARMACIST.’ Set a reminder. Do it.
Jessica Adelle
November 6, 2025 AT 05:46This post is an affront to medical professionalism. The casual tone, the emotive anecdotes, the lack of peer-reviewed citations - it is deeply irresponsible to present clinical pharmacology as if it were a TikTok trend. One must not reduce life-saving protocols to emotionally manipulative narratives. The integrity of medical science is being eroded by this performative, populist approach to health communication.
Emily Barfield
November 6, 2025 AT 14:41What if the real question isn’t ‘how do we stop the interaction’… but ‘why do we still rely on a drug that’s this fragile?’
Tacrolimus is like a house of cards built on a single enzyme… and we put it in the hands of people who are already fighting to stay alive?
Isn’t that… kind of monstrous?
And yet - we praise the doctors who manage it… and never ask why the system demands such precision from people who are already broken?
Why don’t we build better systems instead of training patients to be pharmacists?
…I think we’ve forgotten that medicine should heal… not just manage collapse.
Sai Ahmed
November 7, 2025 AT 19:23India has this problem too. But here, they just give you amphotericin B and hope you don’t die. No monitoring. No protocols. My uncle’s creatinine went to 8.4. They said ‘wait and see.’ He’s fine now. Maybe God helped.
Also, why are all these studies from US/EU? Do people in Africa just not get transplants? Or do they just die quietly?
Albert Schueller
November 9, 2025 AT 05:08Interesting post… though I must note several typographical errors (e.g., ‘spike’ misspelled as ‘spike’ in paragraph 3). Also, the claim that ‘15-20% of kidney damage is due to azoles’ lacks a primary source. This feels like an article written by someone who read a Medscape summary and got excited. I’d like to see the actual clinical trial data before I trust this.
Ted Carr
November 10, 2025 AT 03:21So let me get this straight - we have a $100,000 organ transplant… and the solution to a preventable drug interaction is… *checking a drug interaction checker*?
Wow. Groundbreaking.
Meanwhile, in Sweden, they just use micafungin and call it a day. No drama. No dialysis. Just… common sense.
Guess we’re still stuck in the ‘American medical theater’ where profit > prevention.
Bravo.
Rebecca Parkos
November 10, 2025 AT 19:50I’m a transplant nurse. I’ve seen this. I’ve held someone’s hand while their creatinine spiked from 1.2 to 5.8 in 36 hours. I’ve watched families cry because their ‘simple antifungal’ turned their transplant into a death sentence.
Every single one of these cases was preventable.
And yet - we still don’t have universal protocols.
So yes - I’m angry.
And yes - I’m screaming this from the rooftops.
Check your interactions.
Don’t wait for someone to die to care.