Analgesic Nephropathy: How NSAIDs Damage Kidneys and What to Use Instead
 Jan, 8 2026
Jan, 8 2026
Most people think of painkillers as harmless-something you grab off the shelf when your head hurts or your back flares up. But if you’ve been taking them daily for years, you could be quietly damaging your kidneys without knowing it. This isn’t rare. It’s called analgesic nephropathy, and it’s one of the most preventable causes of chronic kidney disease you’ve never heard of.
What Exactly Is Analgesic Nephropathy?
Analgesic nephropathy is kidney damage caused by long-term, high-dose use of pain medications-especially NSAIDs like ibuprofen, naproxen, and aspirin, and sometimes acetaminophen. It doesn’t happen overnight. It builds up over years, often without symptoms until the damage is advanced.
The kidneys filter blood and regulate fluid balance. When you take large amounts of NSAIDs regularly, they reduce blood flow to the kidneys by blocking prostaglandins-chemicals that help keep kidney blood vessels open. Less blood flow means less oxygen, more oxidative stress, and eventually, scarring in the inner parts of the kidney called the renal papillae. Over time, this leads to chronic tubulointerstitial nephritis, a slow, silent breakdown of kidney tissue.
Back in the 1970s and 80s, this condition was common because many over-the-counter pain relievers contained phenacetin, a now-banned ingredient linked to severe kidney damage and even cancer. After phenacetin was pulled from the market, cases dropped sharply. But today, the problem hasn’t gone away-it’s just changed shape. Now, it’s mostly from people taking multiple NSAIDs daily, often in combination with acetaminophen or caffeine, for headaches, arthritis, or menstrual pain.
Who’s at Risk?
You don’t have to be taking pills nonstop to be at risk. The real danger zone starts at 6 or more painkillers a day for 3 or more years. That’s not even that unusual. Think about someone who takes two Excedrin Migraine tablets every time they get a headache-three times a week. That’s 6 pills a week. In a year, that’s over 300 pills. In five years? Over 1,500. And many of these pills contain caffeine or codeine, which make the kidney damage worse.
Women between 35 and 55 are most affected-nearly 72% of cases. Why? Chronic headaches, migraines, and menstrual pain are often managed with daily OTC meds. Many women don’t realize they’re crossing the line into dangerous territory. Older adults over 45 are also at higher risk, especially if they have high blood pressure, diabetes, or already have reduced kidney function.
And here’s the scary part: 62% of people diagnosed with analgesic nephropathy say they never thought OTC painkillers could hurt their kidneys. They assumed “over-the-counter” meant “safe forever.” That misconception is what keeps this condition alive.
How Do You Know If It’s Happening to You?
The worst part? There are usually no symptoms at first. No pain. No swelling. No warning signs. The first clue is often a routine blood test showing elevated creatinine-or a dipstick urine test revealing protein in the urine. By the time you feel tired, notice swelling in your legs, or develop high blood pressure, the damage is already significant.
Advanced cases show signs like:
- Flank pain (side or back pain near the kidneys)
- Blood in the urine
- Passing tissue fragments in urine (pieces of dead kidney papillae)
- Anemia from reduced kidney hormone production
- Inability to concentrate urine (frequent nighttime urination)
Doctors use noncontrast CT scans to spot calcifications in the renal papillae-a hallmark sign with 97% specificity. But the best tool is simply awareness. If you’ve been taking painkillers daily for years, ask your doctor for a simple eGFR blood test. It’s quick, cheap, and could save your kidneys.
NSAIDs vs. Acetaminophen: Which Is Worse?
Many people switch from NSAIDs to acetaminophen thinking it’s safer for the kidneys. It’s a common assumption-but it’s not entirely true.
NSAIDs directly reduce kidney blood flow. That’s their main risk. Acetaminophen doesn’t do that. But here’s what the data shows: taking more than 4,000 mg of acetaminophen daily for five years or more increases your risk of chronic kidney disease by 68% compared to non-users. That’s not a small risk. It’s a silent one.
And combination products? They’re the real killers. Pills that mix acetaminophen, aspirin, and caffeine-like Excedrin-have been shown to be 3.7 times more likely to cause kidney damage than single-ingredient pills. Caffeine makes the painkiller work faster, but it also constricts blood vessels, adding more stress to the kidneys. Codeine adds another layer of risk because it’s metabolized in the liver and kidneys, increasing overall toxic load.
So if you’re taking a combo pill daily, you’re not being smart-you’re being at risk.
What Should You Use Instead?
Stopping NSAIDs cold turkey can leave you in pain-and that’s why many people don’t quit. But there are safer, effective alternatives.
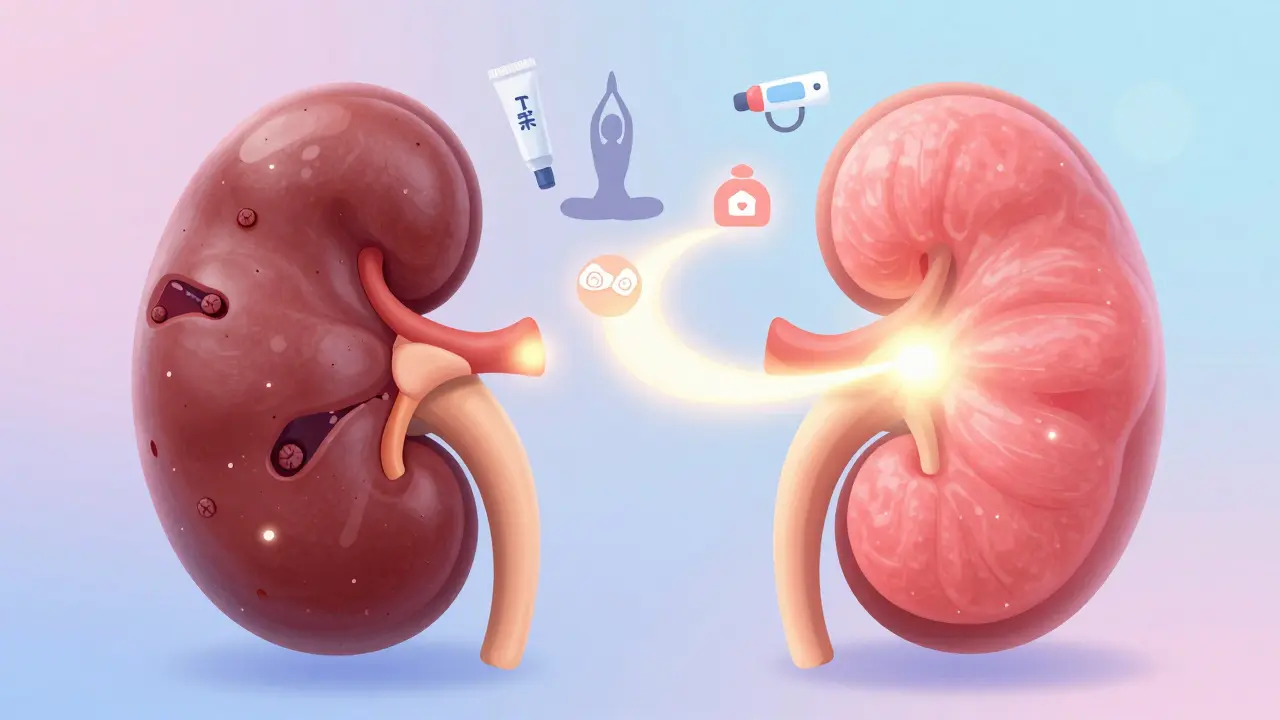
Topical NSAIDs (gels, patches, creams) are one of the best options. A 2021 study showed they deliver the same pain relief as oral pills for osteoarthritis-but with 90% less drug entering your bloodstream. No kidney stress. No stomach issues. Just targeted relief.
Heat therapy works surprisingly well. Devices like ThermaCare HeatWraps have FDA clearance for pain relief without drugs. In clinical trials, they reduced osteoarthritis pain by 40-60%. Heat improves blood flow, relaxes muscles, and doesn’t touch your kidneys at all.
Physical therapy and CBT are now recommended as first-line treatments by the American College of Rheumatology. For chronic back pain, headaches, or joint pain, movement and mindset training often reduce pain more than pills ever could. A 6-week PT program can cut NSAID use by half in many patients.
For migraines, newer prescription options like CGRP inhibitors (e.g., Aimovig, Emgality) are highly effective and carry zero kidney risk. Yes, they’re expensive-around $650 a month-but if you’re already risking your kidneys, it’s worth discussing with your doctor.
And for mild pain? Try non-drug tricks: magnesium supplements for muscle cramps, ginger tea for inflammation, or even acupuncture. These won’t cure everything, but they reduce your reliance on pills.
How to Protect Your Kidneys Now
If you’ve been taking painkillers regularly, here’s your action plan:
- Count your pills. How many NSAIDs or acetaminophen tablets do you take per week? If it’s more than 3 days a week, you’re in the danger zone.
- Stop combo pills. Ditch Excedrin, Anacin, and similar mixtures. Use single-ingredient products only.
- Cap acetaminophen at 3,000 mg/day. That’s 6 extra-strength tablets. Never hit 4,000 mg.
- Use topical NSAIDs. For joint or muscle pain, try Voltaren Gel or similar products.
- Get tested. Ask your doctor for a serum creatinine test and eGFR. Do it every 6 months if you’re on long-term pain meds.
- Find alternatives. Try heat, stretching, physical therapy, or mindfulness techniques before reaching for a pill.
The National Kidney Foundation says no one should take NSAIDs daily for more than 10 days without medical supervision. That’s not a suggestion-it’s a guideline for safety. If you need pain relief longer than that, your doctor should be monitoring your kidney function.
What Happens If You Stop?
Good news: if caught early, the damage can stop. A 2022 study followed 142 people who stopped all painkillers after being diagnosed with early-stage analgesic nephropathy. After five years, 73% had stable kidney function-no further decline. That’s huge. It means your kidneys can heal, if you give them a chance.
But if you keep going? The risk of needing dialysis or a transplant rises. In the U.S., analgesic nephropathy causes 15,000 to 20,000 new chronic kidney disease cases every year. That’s thousands of people who could have avoided this with a simple change in habits.
One patient on Reddit summed it up: “I took 8-10 Excedrin a day for 7 years. My GFR dropped to 45. My nephrologist said I was lucky it wasn’t worse-many people need dialysis from this.”
You don’t have to be one of them.
Final Thought: Pain Isn’t Worth Losing Your Kidneys
Chronic pain is real. It’s exhausting. It changes your life. But you don’t have to numb it into oblivion with pills that slowly kill your kidneys. The solution isn’t stronger drugs-it’s smarter pain management.
Start by tracking your painkiller use. Cut out combos. Try heat or physical therapy. Talk to your doctor about alternatives. Your kidneys won’t thank you today-but they’ll thank you in five years.
Can over-the-counter painkillers really cause kidney damage?
Yes. Taking NSAIDs like ibuprofen or naproxen daily for three or more years, especially in high doses or in combination with acetaminophen or caffeine, can lead to chronic kidney damage called analgesic nephropathy. Even acetaminophen, often seen as safer, can harm kidneys if taken over 3,000 mg daily for five or more years.
How do I know if I have analgesic nephropathy?
Early stages usually have no symptoms. The first sign is often an abnormal blood test showing elevated creatinine or a low eGFR. Urine tests may show protein or sterile pyuria. If you’ve been taking painkillers daily for years and have unexplained fatigue, swelling, or high blood pressure, ask your doctor for a kidney function test.
Is acetaminophen safer than NSAIDs for kidneys?
Acetaminophen doesn’t reduce kidney blood flow like NSAIDs do, so it’s generally safer. But taking more than 3,000 mg daily for five or more years still increases chronic kidney disease risk by 68%. Combination pills with acetaminophen, aspirin, and caffeine are especially dangerous.
What’s the best alternative to NSAIDs for chronic pain?
Topical NSAID gels (like Voltaren) reduce systemic exposure by 90% and are very effective for joint and muscle pain. Heat therapy devices like ThermaCare HeatWraps also offer strong pain relief without kidney risk. Physical therapy, cognitive behavioral therapy, and movement-based treatments are now recommended as first-line options for chronic pain.
Can kidney damage from painkillers be reversed?
If caught early, yes. Stopping all painkillers and managing risk factors like blood pressure and diabetes can halt further damage. In one study, 73% of patients who stopped NSAIDs and acetaminophen showed no further decline in kidney function over five years. The kidneys can stabilize-even heal partially-if the stress is removed.
How often should I get my kidneys checked if I take painkillers regularly?
If you take NSAIDs or acetaminophen more than three days a week, get a serum creatinine and eGFR test every six months. If you have other risk factors-like high blood pressure, diabetes, or existing kidney disease-your doctor may recommend monthly checks during the first six months of ongoing use.
Angela Stanton
January 10, 2026 AT 08:13Okay but let’s be real - if you’re taking 8-10 Excedrin a day for 7 years, you’re not managing pain, you’re self-medicating trauma. 🤯 NSAIDs + caffeine + acetaminophen is basically a kidney demolition derby. The fact that this is still OTC is a public health failure. My nephrologist called it ‘slow-motion suicide’ and I didn’t even realize I was doing it until my eGFR hit 48. Now I use Voltaren gel, heat wraps, and cryotherapy. No pills. No regrets. 🧊💪
Kiruthiga Udayakumar
January 10, 2026 AT 13:36People like you think you're being clever by switching to 'safer' meds, but you're just swapping one poison for another. Acetaminophen isn't safe - it's a silent killer. And don't even get me started on those who think 'natural remedies' fix everything. Ginger tea won't save your kidneys if you're still popping pills like candy. Stop being naive. This isn't a wellness blog - it's a warning. 🚨
Maggie Noe
January 11, 2026 AT 13:57It’s funny how we treat pain like a problem to be erased rather than a signal to be understood. 🤔 We’ve built a culture where discomfort is the enemy - not the teacher. If your body’s screaming for rest, movement, or emotional release, no pill will fix that. The real question isn’t ‘which drug is least toxic?’ - it’s ‘why am I in so much pain that I need daily chemical escape?’ Maybe the kidneys aren’t the problem. Maybe they’re the messengers. 🌱
Heather Wilson
January 12, 2026 AT 12:33According to the National Kidney Foundation guidelines, NSAID use beyond 10 days without medical supervision is contraindicated. Yet, 72% of patients with analgesic nephropathy report no prior physician consultation. The data is clear. The clinical evidence is overwhelming. The failure is systemic - not individual. This isn’t about willpower. It’s about access to care, pharmaceutical marketing, and the normalization of self-medication in a capitalist healthcare system. You can’t fix this with memes or heat wraps. You need policy change. And until then, people will keep dying quietly.
Micheal Murdoch
January 12, 2026 AT 22:35Hey - if you’re reading this and you’ve been taking painkillers daily, don’t panic. You’re not broken. You’re just human. The fact that you’re here means you care. Start small: track your pills for a week. Swap one combo pill for a heat wrap. Talk to your doc about eGFR. You don’t have to go cold turkey - just go *mindful*. I’ve seen patients reverse early-stage damage just by cutting back and adding stretching. Your kidneys aren’t doomed. They’re just waiting for you to give them a break. You’ve got this. 💪
Johanna Baxter
January 14, 2026 AT 19:38I took 12 Excedrin a week for 10 years and now I’m on dialysis. No one warned me. My mom said ‘it’s just aspirin.’ My doctor said ‘it’s fine.’ I trusted everyone. Now I can’t even hug my grandkids without being exhausted. Don’t be like me. Stop. Now. 💔
Patty Walters
January 16, 2026 AT 18:23just wanted to say i started using topical ketoprofen gel after my dr told me my creatinine was up - no more stomach burns, no more kidney stress, and my knee pain actually improved? weird right? also switched to magnesium glycinate for cramps and cut caffeine. no more combo pills. i’m not ‘healed’ but i’m not dying either. small wins. 🙏
Phil Kemling
January 18, 2026 AT 14:42What’s the cost of silence? We numb pain because we’re afraid of what’s underneath - grief, burnout, trauma, loneliness. The kidneys don’t lie. They reflect what we refuse to feel. Maybe the real analgesic isn’t a pill - it’s presence. With ourselves. With others. With the quiet ache we’ve been trained to fear. Healing isn’t always about fixing. Sometimes it’s about listening.